Answer of November 2010
Clinical History:
A 72-year-old gentleman with history of gallstones was presented with abdominal pain for 2 days. He was found to be hypotensive and blood tests revealed severe metabolic acidosis with pH 7.16, HCO3 6.8. White cell count was 24. Amylase was 1500. Urgent CT of the abdomen with contrast was performed.
Diagnosis:
Infected necrosis complicating pancreatitis
Discussion:
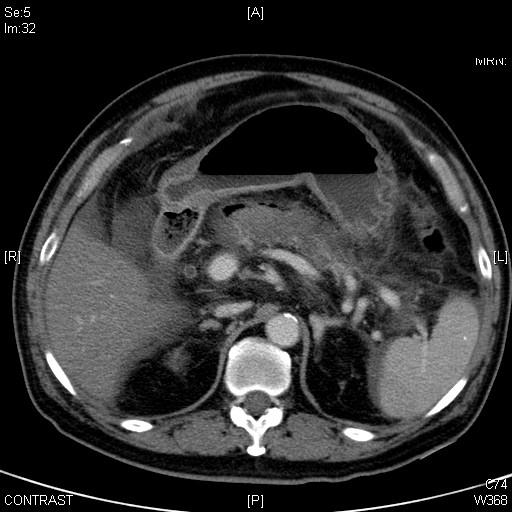
CT of this patient reveals a swollen pancreas with heterogeneous hypoattenuation and indistinct margins. Absence of normal parenchymal enhancement is demonstrated in the majority of the pancreatic gland. Pockets of gas are found over the anterior surface of body and around the tail. Features are suggestive of necrotising pancreatitis with superimposed infection.
Gallstones and alcohol abuse are the most common causes of acute pancreatitis, accounting for 80% of cases. 80-85% of cases of acute pancreatitis run a mild course. This group of patients has a mortality of < 1%. 15-20% of cases of acute pancreatitis run a serious clinical course with pancreatic necrosis and the development of multiple organ failure. Of these, pancreatic necrosis remains sterile in 60% of patients, whereas in 40% of these patients the necrosis becomes infected. This category of patients has the highest mortality rate of 25-70%.
Severe acute pancreatitis or necrotizing pancreatitis runs a biphasic course. During the first 1-2 weeks there is a pro-inflammatory response, resulting in a systemic inflammatory response syndrome (SIRS) which is a sterile response. After the first 1-2 weeks there is a transition from a pro-inflammatory to an anti-inflammatory response. It is during this anti-inflammatory response that the patient is at risk for the translocation of intestinal flora and the development of infection of necrotic tissue and fluid collections. The subsequent sepsis will result in late multiple organ failure.
In necrotizing pancreatitis, lack of enhancement of the normal pancreatic tissue can be demonstrated in contrast CT. The detection of pancreatic necrosis in clinical practice is important because most life-threatening complications occur in patients with pancreatic necrosis.
30-70% of patients with acute necrotizing pancreatitis develop local pancreatic infection, which has near 50% mortality even with surgical debridement.
Infected necrosis usually occurs in the second and third week, air bubbles can be demonstrated in CT in 20% of cases with infected necrosis. Risk of infection increases with the amount of necrosis and the time from onset of pancreatitis.
Benefit of surgery in patients with sterile necrosis remains unproven but should be pursued in cases with multi-organ failure unresponsive to medical treatment. Infected necrosis is a clear indication for necrosectomy. Percutaneous drainage generally fails to be curative but may be beneficial in stabilizing septic patients.
This patient underwent emergency operation for necrosectomy on the same day, intreoperatively they found the whole pancreas looked haemorrhagic with necrosis mainly in head and neck region. There was also gross retroperitoneal haemorrhagic swelling. Patient died the next day.