Answer of August 2011
Clinical History:
An 11 years old girl presented with recurrent swelling at right parotid region for a few months (about 7 episodes in 6 months). The size of swelling fluctuated throughout each episode, but never returns to normal during the quiescent periods. Her oral hygiene was satisfactory and there was no history of dental caries or extraction. The episodes were not associated with febrile illness. Initial ultrasound examination of the parotid gland showed no focal mass, stone or dilated ductules. Contrast CT scan of the face was eventually arranged for the provisional clinical diagnosis of recurrent parotitis. X-rays were taken after the CT examination.
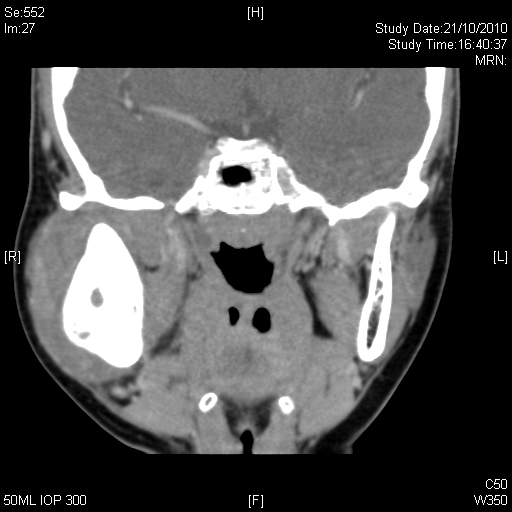
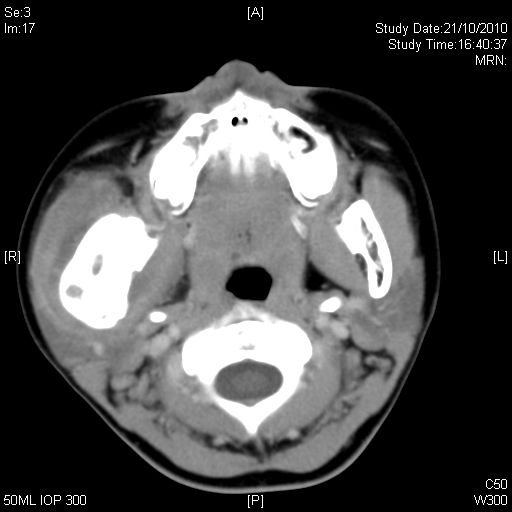
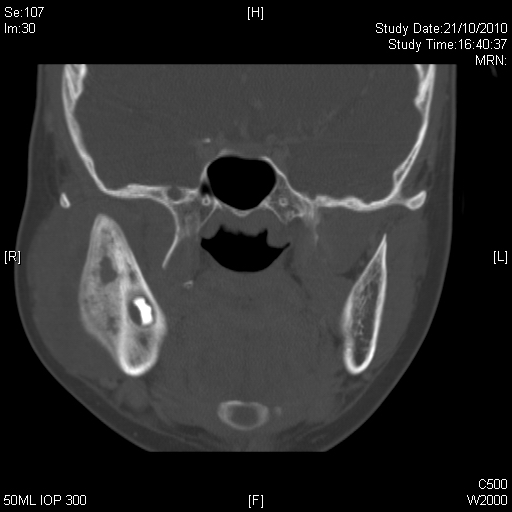
Post-contrast CT images
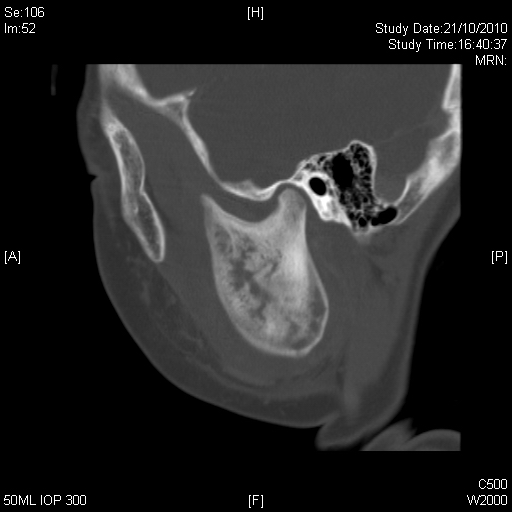
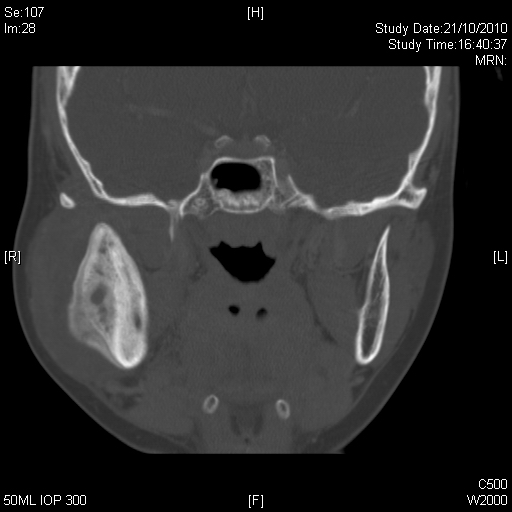
Coronal and sagittal CT images (Bone window):
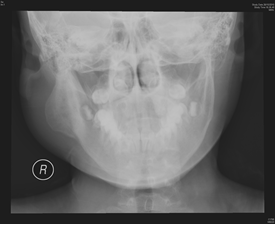
Plain radiograph of the mandible
Diagnosis:
Garre's Osteomyelitis
Discussion:
Garre's osteomyelitis is also known as periostitis ossificans, non-suppurative chronic osteomyelitis, and chronic osteomyelitis with proliferative periostitis. It is a distinctive type of chronic osteomyelitis associated with intense proliferation of periosteum and reactive peripheral lamellar bone formation caused by a slight irritation or mild infection, without necrosis or purulent exudate.
The condition is seen exclusively in children or young adults. Mandible is more often affected than the maxilla. This entity is well described in the dental literature and is usually associated with dental caries. Other causative factors have been reported, such as dental extraction, mild periodontitis, tooth follicles, periodontitis associated with an ectopically erupting posterior molar, and other non-odontogenic cause (e.g. spread from pharyngitis); while some cases were of unknown aetiology. Its occurrence is rare, because its development depends on the integration of conditions: a chronic infection in an individual, usually a young person, with a periosteum capable of vigorous osteoblastic activity, and the equilibrium between the virulence of the infectious agents and the resistance of the host. Clinically it can manifest as a bony hard, non-tender swelling which is slowly progressive, and may be associated with a painful carious tooth. A presentation of regional painful swelling that resembled a facial abscess was also described. This case presented with episodic flaring with subsequent partial resolution.
Garre's osteomyelitis should be distinguished from infantile cortical hyperostosis which occurs in young infants and involves a number of bones (e.g. clavicle and ulna). Other differential diagnoses would include Ewing's sarcoma, osteosarcoma, fibrous dysplasia, cherubism, hypertrophic osteoarthropathy, syphilitic osteomyelitis, healing fracture, Langerhans cell histiocytosis, and pyogenic or tuberculous osteomyelitis. E-wing sarcoma and osteosarcoma have more aggressive growth pattern and may be associated with osteolysis and soft tissue involvement. Sclerotic change / new bone formation in fibrous dysplasia is typically endosteal. Cherubism is bilateral and generally involves the maxilla. Hypertrophic osteoarthropathy is unusual in children and is centered at the temporomandibular joint. Diagnosis of Langerhans cell histiocytosis is difficult and biopsy is often required.
The treatment strategy is to remove the cause, and aided by an adequate antibiotic therapy. Surgical procedures such as periodontal surgery, tooth extraction, or additional curettage of the socket, may be required. Surgical re-contouring of the cortical expansion is usually not required, because the jaw may gradually remodel during the remained growth period.