Answer of April 2011
Clinical History:
A 24-year-old lady with multiple episodes of epitaxis.
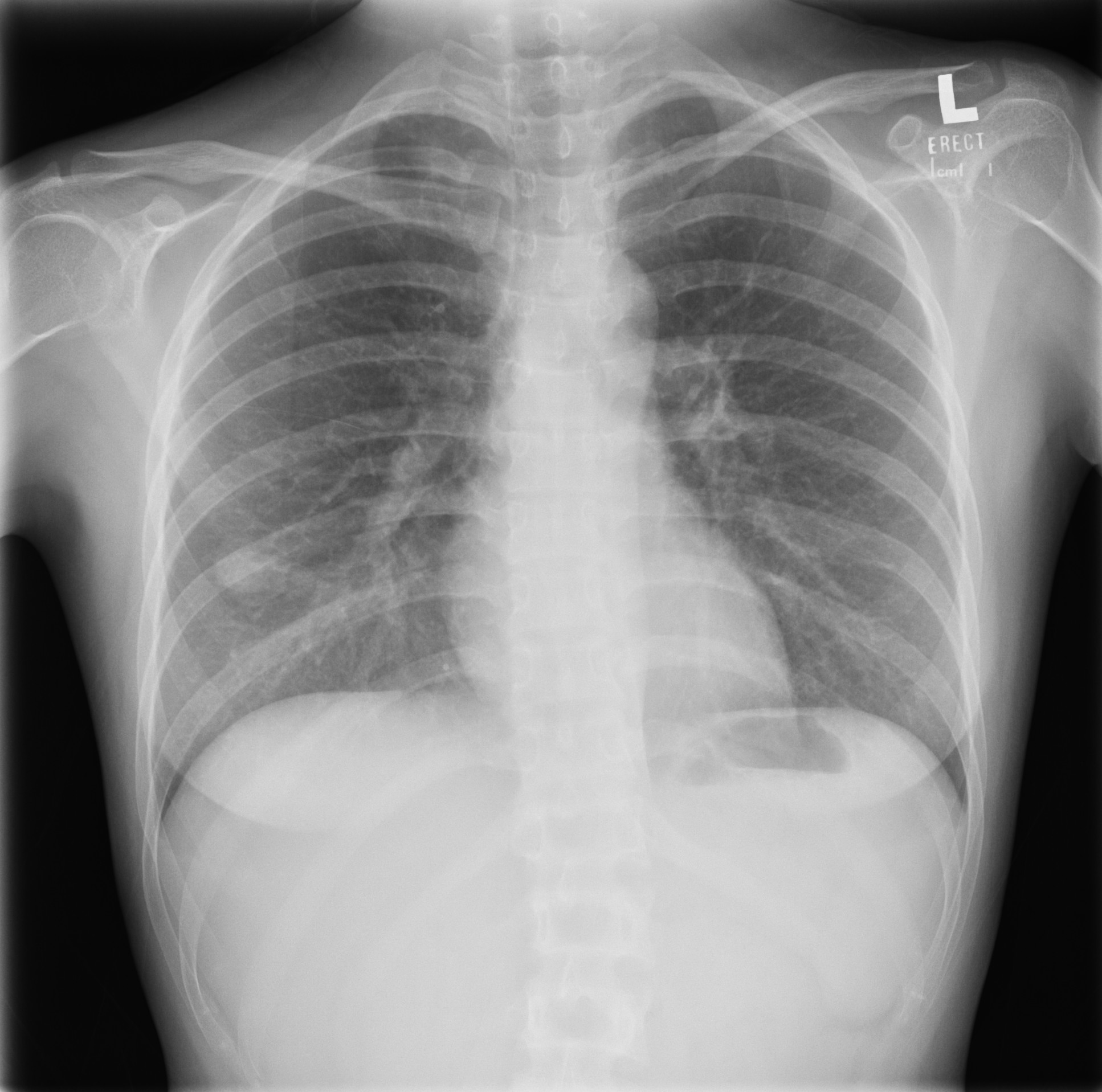
CT thorax performed for further
workup of the right lower
zone lung nodule
Diagnosis:
Hereditary Hemorrhagic Telangiectasia (Osler-Weber-Rendu Disease)
Discussion:
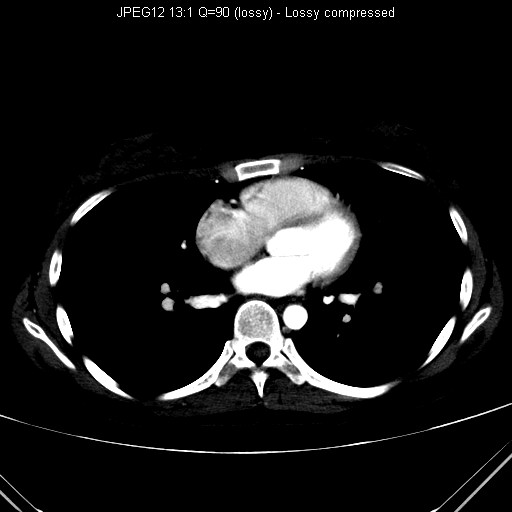
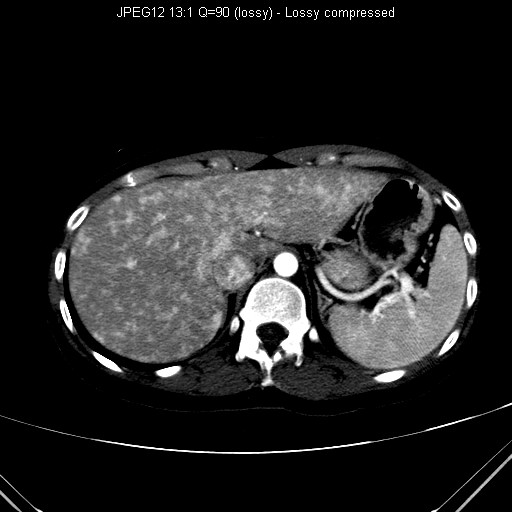
Hereditary Hemorrhagic Telangiectasia is a rare autosomal dominant disease with variable penetrance. It is characterized by the presence of teclangiectasia and arteriovenous malformations (AVMs) in multiple organs. Classical features include recurrent epistaxis (most common presentation), telangiectasias (typically less than 0.5cm), positive family history, and multiorgan AVMs and aneurysms. Symptoms are related to bleeding or shunting from these AVMs. Overall, 30-50% patients with pulmonary AVMs have HHT while only 20% patients of HHT have a pulmonary AVM. Pulmonary AVMs usually appear as lobulated well defined masses with cord like extensions to the pulmonary vessels. Around 36% of pulmonary AVMs in HHT are multiple and 50% are bilateral. Pulmonary AVMs allow the emboli from the venous system to bypass the normal pulmonary capillary filtering and reach the systemic circulation, causing ischemia or septic emboli. At the brain, intracranial haemorrhage could be resulted from cerebral AVMs while ischemic infarction, septic emboli and brain abscesses are related to pulmonary AVMs. The liver is involved in 10-30% of HHT patients with variable radiological presentations include teclangiectases, large confluent vascular masses, perfusion abnormalities etc. Large hepatic AVMs could be complicated with high output cardiac failure. Embolization or ligation may be used on pulmonary or hepatic AVMs while bowel resection might be required in case of gastrointestinal haemorrhage.