Answer of March 2011
Clinical History:
A 10-year-old boy was admitted because of acute onset of right scrotal pain for three hours. He did not have the history of trauma, dysuria or fever. Physical examination found tenderness over the right testis, mildly swollen and erythematous right hemiscrotum.
Diagnosis:
Acute torsion of the right testis
Discussion:
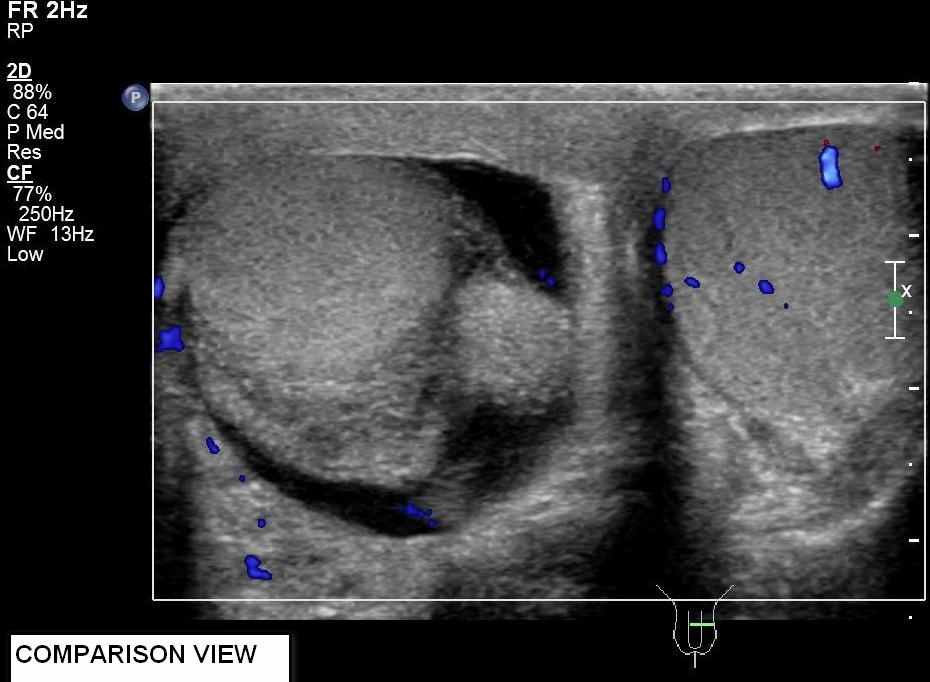
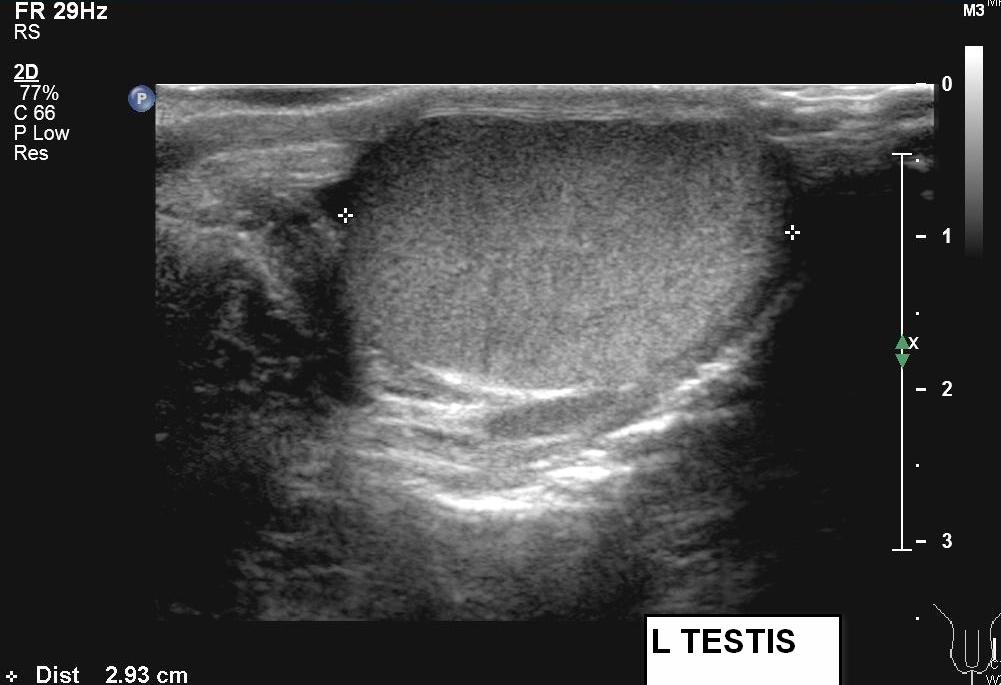
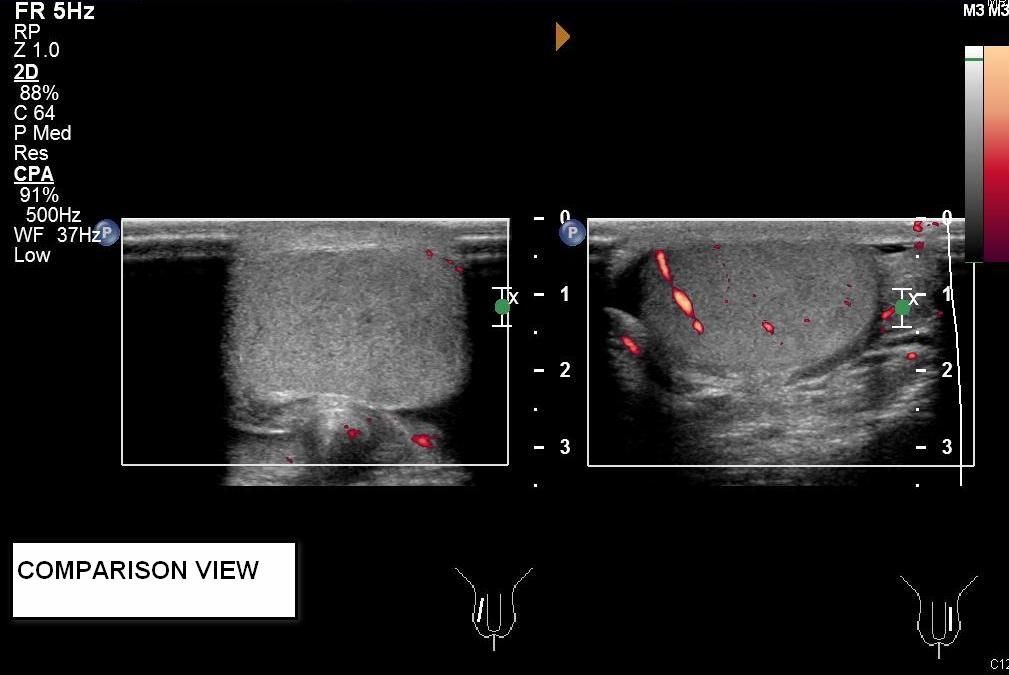
Greyscale ultrasound showed small amount of right hydrocele and swollen right epididymis. Both testes had normal echopattern and smooth outline. Color and power Doppler ultrasound studies showed absence of intratesticular blood flow on the right side. Perfusion over the left testis was normal. Findings were compatible with acute right testicular torsion.
Testicular torsion is a urological emergency. Prompt diagnosis is essential. The salvage rate of torsed testes is 80-100% when surgery is performed within 6 hours of onset of pain. It significantly drops to 70% and 20% when surgical intervention is contemplated 6-12hours and more than 12 hours after torsion respectively. Clinical symptoms are traditionally used to classify testicular torsion. Acute testicular torsion occurs when symptoms present for less than 24 hours. Subacute testicular torsion, also known as missed torsion, means presentation is between one to ten days of symptom onset. The term chronic testicular torsion applies when symptoms had begun before or persist for more than ten days.
When clinical suspicion of torsion is high, emergency surgery is indicated to maximize the change of testicular salvage. The main clinical dilemma of a child presenting with an acutely painful swollen testis is to distinguish testicular torsion from acute epididymo-orchitis. When physical examination findings are equivocal, ultrasonography with Doppler capabilities is the investigation of the choice.
Greyscale appearance of the testis changes depends on the duration of torsion and severity of compromised blood flow. Testis can appear normal within first few hours of disease onset. Hydrocele and scrotal skin thickening are early findings but they are non specific. As disease progresses, infarct and hemorrhage occur. Testicular swelling and mixed testicular echogenicities are seen. Swollen and echogenic epididymis can be detected. If left untreated, testis will undergo atrophy and even calcification.
Color Doppler ultrasound has a reported sensitivity of 89% and specificity of 100% in diagnosing testicular torsion. [1] With settings optimized to for slow blood flow detection, which include low pulse repetition frequency and a low velocity scale, absence of intra-testicular blood flow on color Doppler imaging is a diagnostic sign. Power Doppler ultrasound, a technique of mapping the magnetic of the backscattered Doppler signal rather than Doppler shifted flow velocities, have been demonstrated to be more sensitive in detecting low flows. It is especially useful to demonstrate intra-testicular blood flow in prepubertal testes [2].
In summary, testicular torsion is a urological emergency. Grey scale ultrasound appearance of the testis can be normal in early stages. Ultrasound with color and preferably power Doppler capabilities is the imaging modality of choice if physical examination findings are equivocal.