Answer of September 2012
Clinical History:
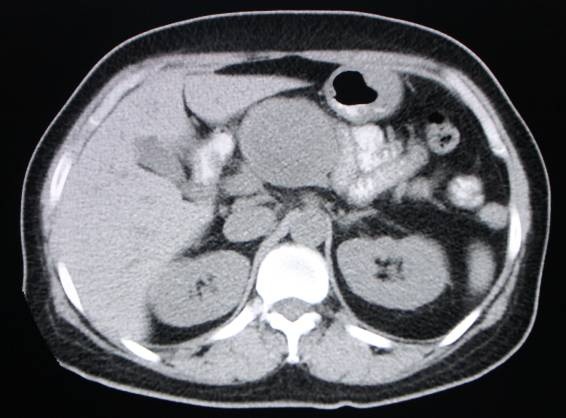
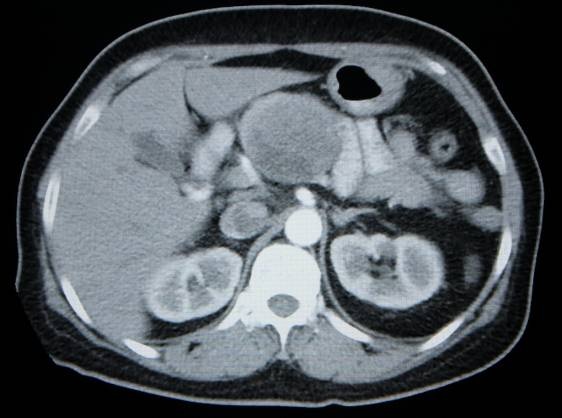
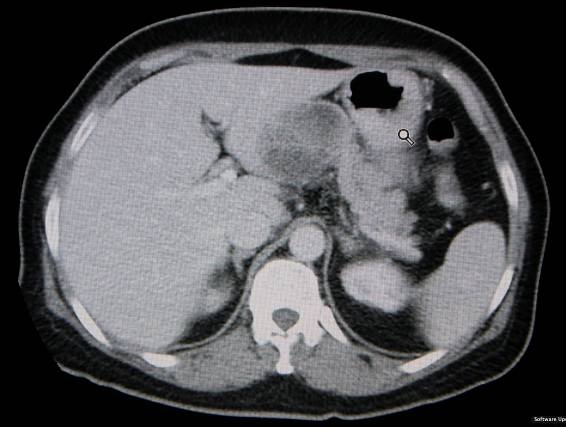
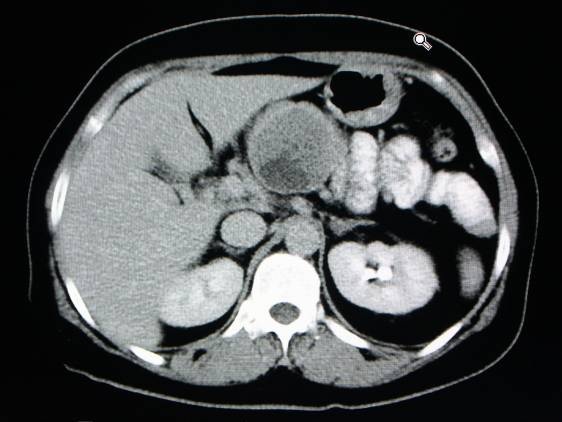
This Asian lady in her forties presented with faintness for a few months and a low haemoglobin count. CT performed for investigation of her anaemia incidentally showed an abnormality in the pancreas.
Diagnosis:
Solid pseudopapillary tumour of the pancreas.
Discussion:
Solid pseudopapillary tumour (SPT) is an uncommon neoplasm of pancreas. It has many synonyms, including solid and cystic tumour, solid and papillary epithelial neoplasm, papillary-cystic neoplasm, and Franz tumour. It was renamed "solid pseudopapillary tumour" by the WHO in 1996.
SPT mainly occurs in non-caucasian (mainly Asian) women of child-bearing age. Characterised by a low potential for malignancy, it has an excellent outcome after complete resection. Typically it remains asymptomatic for long durations, usually found incidentally on imaging performed for other reasons. It may enlarge rapidly during pregnancy due to its positivity for progesterone receptors.
SPTs are typically large at diagnosis (9cm or more), reflecting their asymptomatic nature. They are usually encapsulated, with varying solid and cystic areas - solid areas being more peripheral and cystic spaces being more central. Haemorrhagic components are characteristic. On MRI, areas of high T1W signal and low or inhomogeneous signal on T2W due to blood products are present. Thick fibrous capsule can be seen as a discontinuous rim of low T2W signal. Peripheral heterogeneous enhancement of solid portion with progressive fill-in can be seen post-gadolinium.
Ductal obstruction and liver metastases are uncommon - their presence would signify malignancy.
The main radiological differential diagnosis of SPT is non-functioning islet cell tumour, with which it shares many features - hypervascularity, cystic change, well-defined borders, and lack of desmoplastic reaction. However, haemorrhagic components in solid pseudopapillary tumour are of high T1W signal, whereas cystic areas in islet cell tumour are of intermediate T1W signal. Moreover, non-functioning islet cell tumour typically occurs in elderly patients with no female predominance.