Answer of June 2012
Clinical History:
A 58-year-old lady with end-staged renal failure on hemodialysis for 13 years complained of gradual onset and slowly progressive low back pain for 4 years. She is afebrile all along.
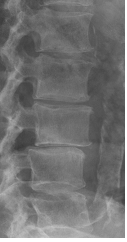
Lumbar spine radiographs
2007 2008 2010
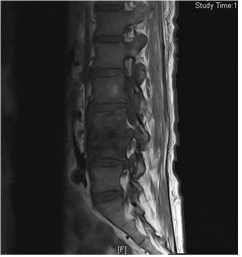
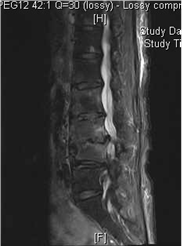
Sagittal T1 MR image Sagittal STIR MR Sagittal STIR MR
image (a) image (b)
Diagnosis:
Destructive spondyloarthropathy associated with dialysis-related amyloidosis
Discussion:
Dialysis-related amyloidosis is a unique type of amyloidosis affecting patients undergoing long-term hemodialysis. It occurs secondarily to the deposition of B2-microglobulin and predominantly involves the osteoarticular system, clinically manifested by erosive and destructive osteoarthropathies, destructive spondyloarthropathy and carpal tunnel syndrome. The visceral (systemic) form has a relatively lower incidence and occurs late in the course of the disease.
Generally, MRI shows decreased T1 signal in the bone lesions. Various signal intensity is noted in T2, due to combination of amyloid deposits and fluid collection within the subchondral lesions. Identification of an intraosseous lesion with relatively low signal on both T1- and T2-weighted images is helpful in the diagnosis of amyloidosis.
In cases of destructive spondyloarthropathy, there is characteristic erosions of anterosuperior and anteroinferior corners of the vertebral body, severe narrowing of the intervertebral disc space, and erosions and cysts of adjacent vertebral plates with minimal osteophyte formation. As the disease progresses, vertebral body collapse, subluxation or listhesis may occur. CT is the best method for detecting small osteolytic areas in cortical bone. MRI can demonstrate amyloid deposits in the disc, synovium and in the ligamentum flavum.
Difficulties may arise in differentiating changes secondary to dialysis-related amyloidosis from spondylodiscitis. In the latter, structures involved show decreased T1, increased T2 and increased STIR signals. In most cases of dialysis-related amyloidosis, low-signal is present in T2-weighted images, allowing exclusion of an infection. For our patient, the disease is slowly progressive disease, rendering the differential diagnosis of infective spondylodiscitis unlikely.
Biopsy is nearly always required for definitive diagnosis. However, because histologic confirmation is not always possible and increased serum B2-microlobulin level is not diagnostic, imaging findings combined with history and clinical findings are usually used for assessment of musculoskeletal involvement.
Treatment is that for enhancing B2-microglobulin clearance, including effcient high-flux dialysis methods, hemofiltration and immunoadsorption. Renal transplantation may help in alleviating osteoarticular symptoms, though regression of amyloid deposits probably does not occur.