Answer of March 2013
Clinical History:
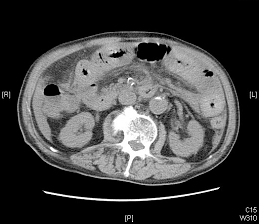
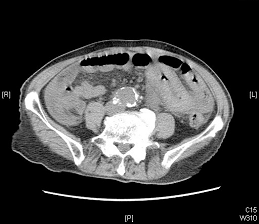
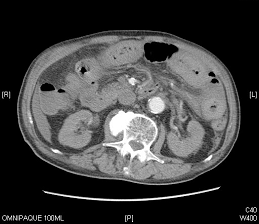
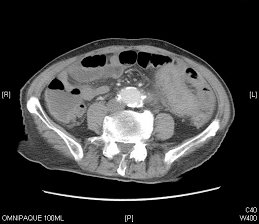
This 85 year-old man, with history of atrial fibrillation and mitral valve replacement on long-term warfarin, was presented with dull lower abdominal pain for 3 days. There was no history of recent trauma. On admission, patient was patient was afebrile. Haematological investigation showed anaemia and prolonged prothrombin time (INR>7). White cell count was mildly elevated. Un-enhanced and contrast-enhanced computed tomography (CT) of abdomen and pelvis was performed as urgent request.
Diagnosis:
Spontaneous small bowel intramural haematoma due to over-anticoagulation with warfarin
Discussion:
Spontaneous intramural small bowel haematoma is an infrequent complication of warfarin anticoagulation, and it is the most common cause of the condition. Other risk factors include hemophilia, idiopathic thrombocytopenic purpura, leukemia, lymphoma, myeloma, chemotherapy, vasculitis, pancreatitis, and pancreatic cancer. Presentation of patients varies from mild and vague abdominal pain to intestinal tract obstruction and an acute abdomen.
Spontaneous small bowel intramural haematoma usually occurs in jejunum, followed by ileum and the duodenum. On the contrary, traumatic small bowel intramural haematoma usually occurs focally in the duodenum and segment of involvement is shorter.
Un-enhanced CT findings include homogeneous and symmetric intramural thickening with hyperdense material (30-80 HU) in the bowel wall. The hyperdensity of the bowel wall can be seen during the first 10 days after the onset of symptoms and can be helpful in distinguishing this condition from other infiltrative processes that can affect the small bowel, such as malignancy and infection.
Complete resolution of the hematoma usually occurs within a few weeks after onset. Those patients with non-extensive small bowel intramural haematoma have good outcome and no bowel resection in needed after adequate medical treatment. Patients with extensive intramural hematomas involving more than half the length of the small intestine may represent an important subgroup with a poor outcome.