Answer of May 2015
For completion of the online quiz, please visit the HKAM iCMECPD website: http://www.icmecpd.hk/
Clinical History:
A 56-year-old female patient of end-stage renal disease on peritoneal dialysis presented with a 6-month history of progressive low back pain. No focal neurological symptom otherwise. The neurological examination was unremarkable.
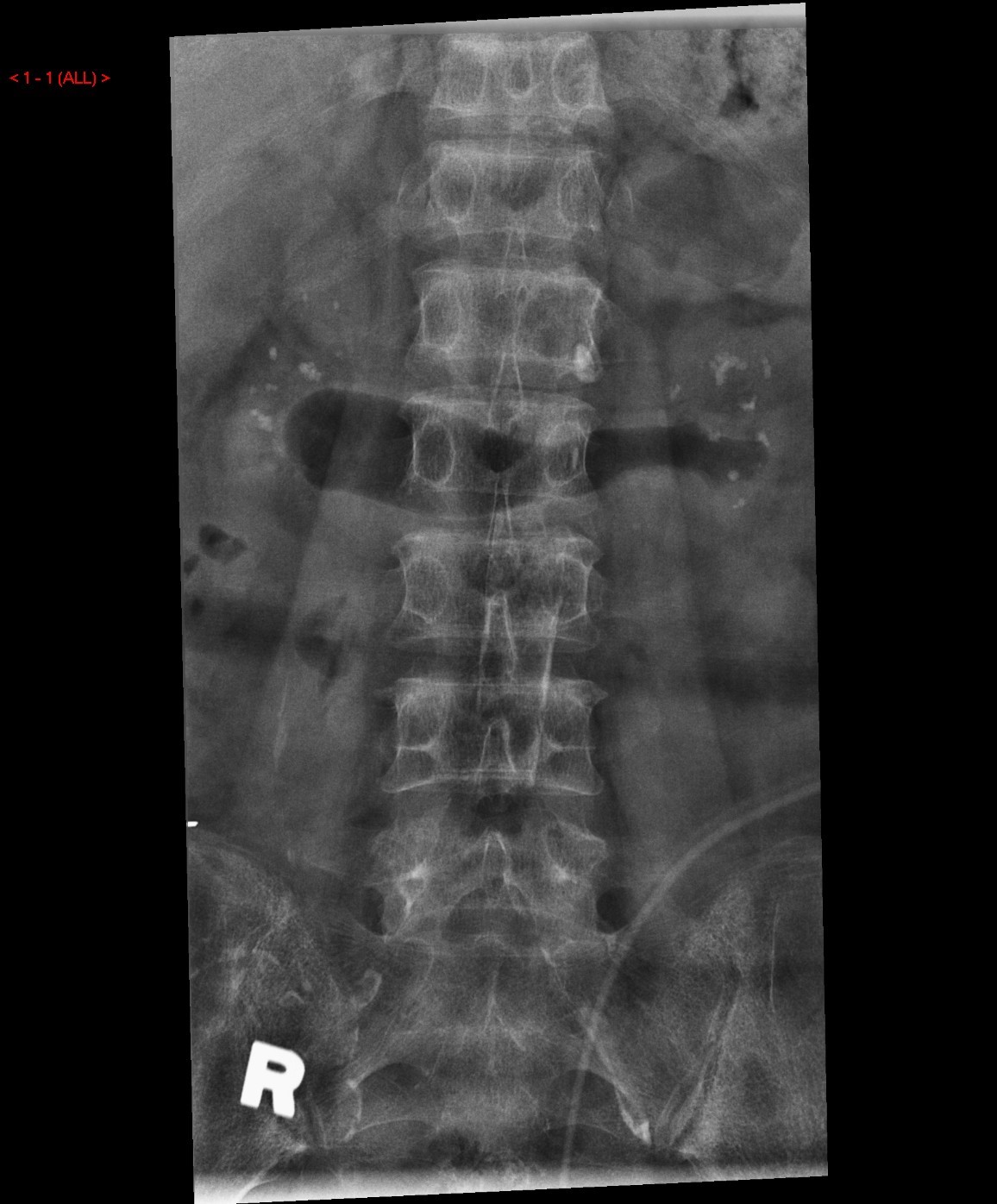
X Rays of lumbosacral spine:
Plain CT Lumbosacral spine:
Selected reformatted images at L1:
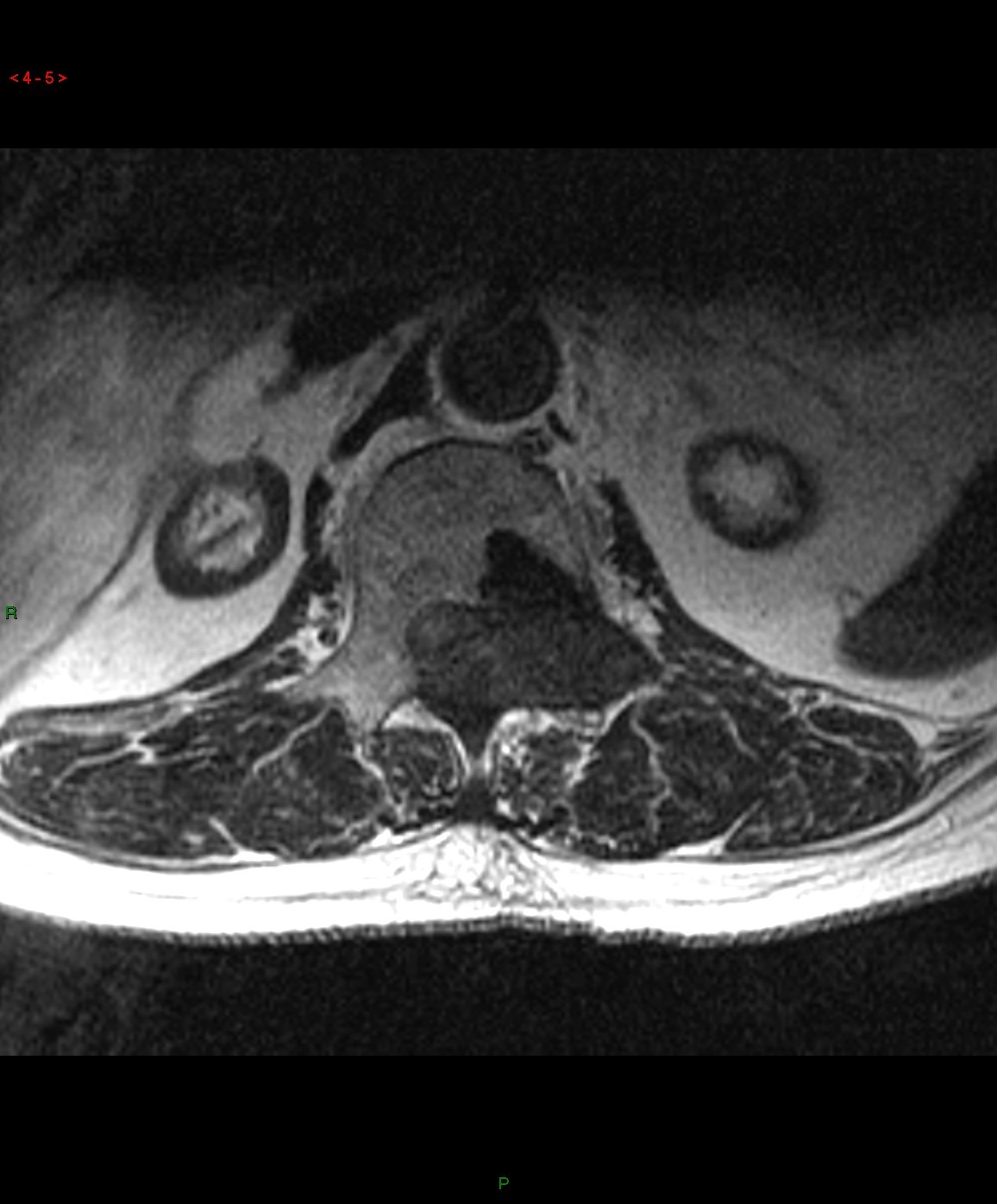
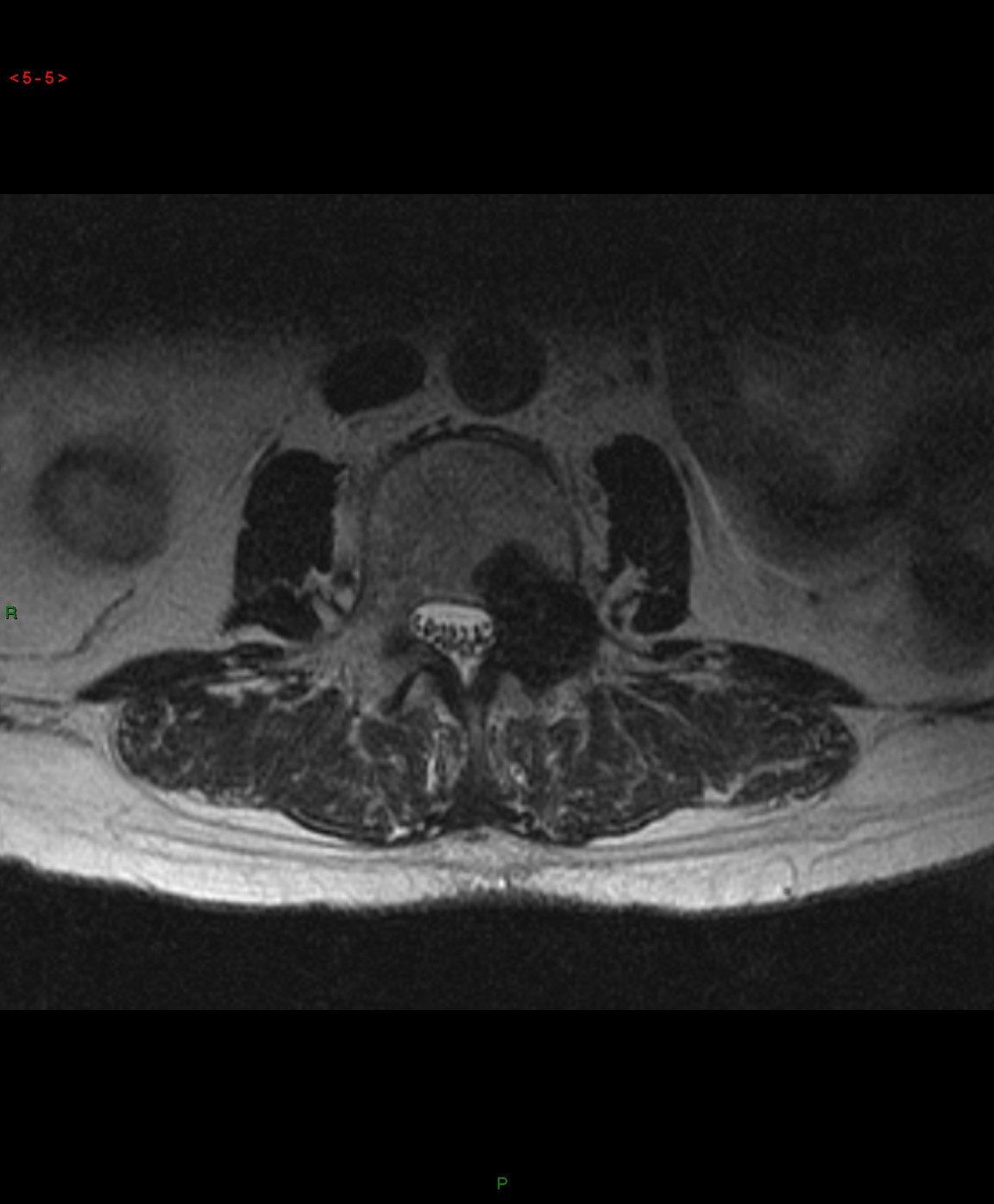
MRI Lumbosacral spine :
Axial T2W images at L1 (LEFT) and L3 (RIGHT) respectively:
DIAGNOSIS:
Brown tumour of the spine resulting in compression of conus medullaris and cauda equina.
DISCUSSION:
While brown tumours of the
appendicular skeleton are well-known to be associated with hyperparathyroidism
(primary > secondary), brown tumour of the spine complicated by cord / cauda
equina compression is very rare. Most
cases reported in literature are associated with chronic renal disease in
adults. The patients may present with
back pain of insidious onset, and progressive weakness related to cord
compression, or acute back pain and paraplegia related to pathological
fractures.
Imaging findings include lytic solitary or
multifocal sharply demarcated expansile lesions on radiographs, CT and MRI. On
bone scan they are MDP-avid and may mimic metastases. Correlation with serum parathyroid hormone
levels, sestamibi scan for parathyroid lesions and other radiographic features
of hyperparathyroidism would be helpful. However, since the differential
diagnoses of these lesions include amyloidosis, metastases and myeloma, which
are much more common in renal patients, the diagnosis of brown tumour should
only be made by exclusion. CT-guided biopsy for
obtaining histological diagnosis is often warranted.
For treatment, the main aim is to optimize
control of the hyperparathyroidism. Like other brown tumours, these spinal
lesions may resolve 1-2 years after subtotal parathyroidectomy. Medical
treatment (eg cinacalcet) alone is often considered inadequate for prevention
of tumour growth or recurrence. Urgent decompression surgery may be warranted
if patients present with acute neurological deficits.