Answer of November 2014
For completion of the online quiz, please visit the HKAM iCMECPD website: http://www.icmecpd.hk/
Clinical History:
44-year-old man presented with on and off headache for 1 year. Ventricular drainage catheter was inserted by neurosurgeon as bilateral papilledema noted. CSF cytology & culture were both negative. No primary tumor or skin pigmentation was identified.
CT (plain) & MRI were performed as part of workup. (axial T1, axial T2, axial T1 post-Gd)
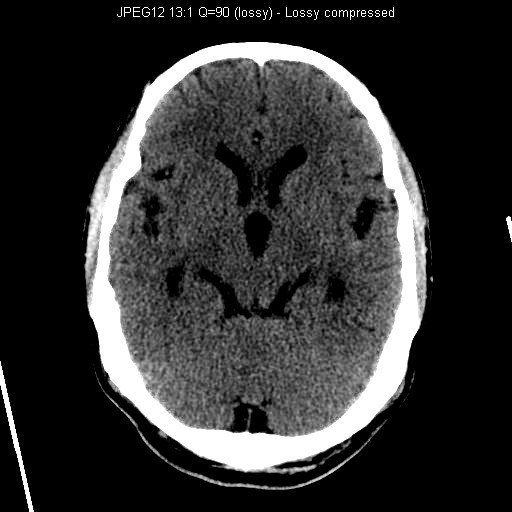
CT Brain (Plain)
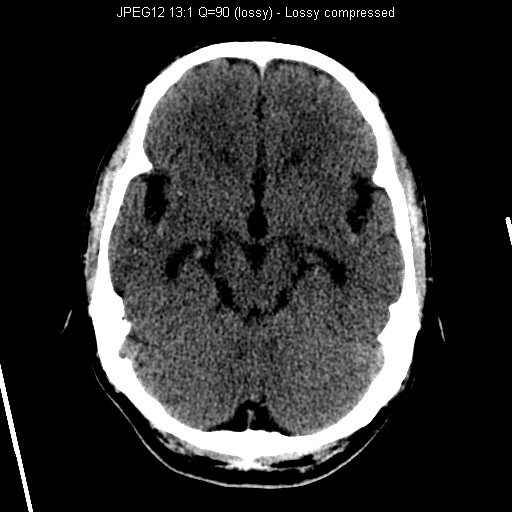
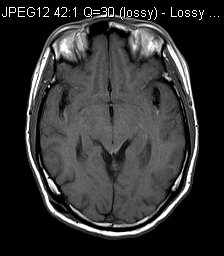
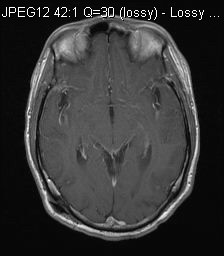
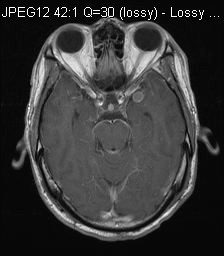
MRI T1W
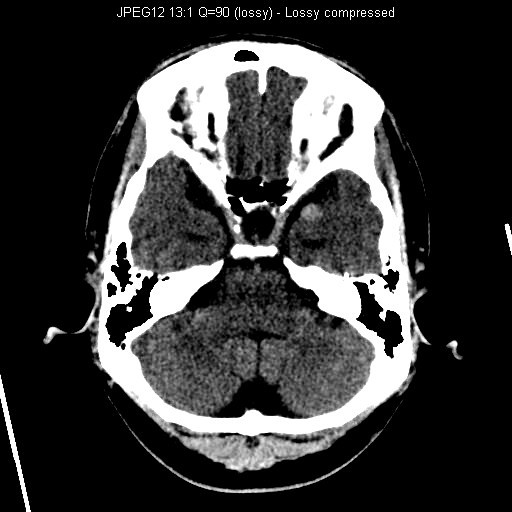
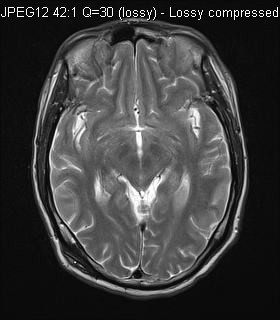
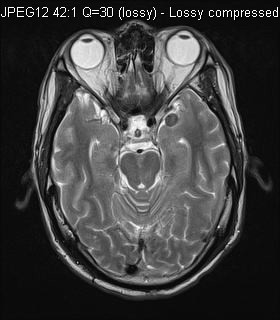
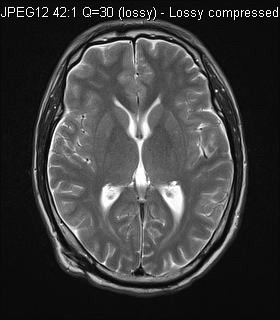
MRI T2W
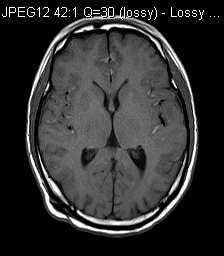
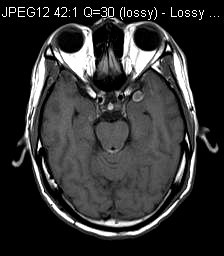
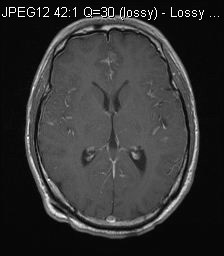
MRI Post-Gd T1W
Diagnosis:
Primary leptomeningeal melanomatosis
Discussion:
CT showed multiple hyperdensities in bilateral Sylvian fissures and extra-axial space of left middle cranial fossa. Ventricular system was dilated.
MRI showed diffuse leptomeningeal enhancement bilaterally, most of them were T1 hyperintense. The one in left middle cranial fossa showed T2 hypointensity. Features were in keeping with primary leptomeningeal melanomatosis.
Differentials for T1 hyperintensity in the subarachnoid space included blood, fat and melanin. Absence of fat density in CT suggested against rupture dermoid cyst. Absence of trauma history and presence of diffuse leptomeningeal enhancement suggested against subarachnoid hemorrhage.
It could be difficult to differentiate between leptomeningeal carcinomatosis and diffuse leptomeningeal melanomatosis. However, absence of primary tumor and T1 hyperintensity made primary leptomeningeal melanomatosis more likely.
Primary leptomeningeal melanomatosis was a rare variant of primary malignant melanoma. It resulted from spread of malignant melanocytes into the leptomeninges and Vircow-Robin spaces, with superficial invasion of brain. This disease was more common in adult. Patients presented with various symptoms include seizure, psychiatric disturbance or signs of raised intracranial pressure. Antemortem diagnosis was difficult. Identification of T1 hyperintensity and diffuse leptomeningeal enhancement served as clues to reach the diagnosis. Brain or meningeal biopsy was usually indicated to confirm the diagnosis, like in our case.