Answer of April 2014
Clinical History:
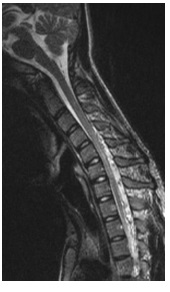
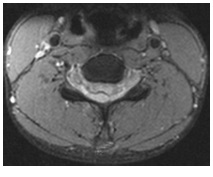
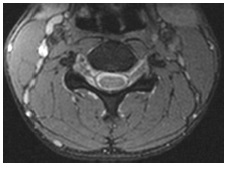
A 19-year-old male presented with bilateral upper limb and lower limb weakness for 1 year. Physical examination showed wasting of hand muscles and features of myelopathic hands. Dynamic MRI was performed (5 images – upper row: T2 weighted sagittal images of cervical spine in extension, flexion and neutral neck positions; lower row : axial T2 weighted axial images of cervical spine in flexion and neutral neck positions.)
Diagnosis:
Hirayama disease
Discussion:
Dynamic flexion MRI showed the characteristic findings of anterior shifting of posterior wall of cervical dural sac, stretching and tightening of dural sac, flattening of the lower cervical cord against vertebra, effacement of subarachnoid space, enlargement of posterior epidural space which forms a crescent shaped mass, prominent epidural flow voids suggestive of epidural venous congestion and enhancement of the epidural space on postcontrast studies.
Hirayama disease (HD) is a rare type of cervical myelopathy related to flexion of the neck characterized by progressive muscular weakness and atrophy of the distal upper limbs most frequently seen in young males (1, 2). HD is thought to be secondary to an abnormal anterior displacement of the posterior dura with secondary compression of the lower cervical spinal cord and chronic injury to the anterior gray matter horns. HD is a benign disorder with a stationary stage after an initial progressive course(1).
Neuroradiological findings include straightening of spine/kyphosis, focal asymmetric lower cervical cord atrophy and/or signal alterations, loss of attachment between the posterior dural sac and lamina in neutral neck position (2) Dynamic flexion MRI, which has a sensitivity of 87%. In doubtful cases full flexion CT-Myelography may be done which has sensitivity of 94% (1, 2).
The pathogenic mechanism is unknown, but the most accepted explanation is that there is an imbalance in growth between the vertebral column and spinal canal contents, causing neck flexion–induced myelopathy. The spinal dura mater is attached to the periosteum at two ends: proximally at the foramen magnum and dorsal surfaces of C2 and C3, and distally at the coccyx. The rest of the dura mater is loosely suspended inside the vertebral column. Normally, the dura mater is slack when the neck is in the neutral position, and is stretched when the neck is flexed because there is an increase in the overall length of the vertebral canal, but the posterior dura mater still remains abutting the posterior wall of the spinal canal. In patients with Hirayama’s disease, due tothe presumed imbalance in growth between the vertebral
column and the dura, the dura mater is already tighter in the neutral position. During neck flexion, the tightened posterior dura mater detaches from the posterior lamina and compresses the spinal cord against the anterior vertebral column. This compression causes ischaemic changes in the territory of the anterior spinal artery, particularly at C4-C6 levels, and hence the subsequent denervation of the distal upper limb muscles.
Medical treatment in HD patients consists of a cervical collar for 3–4 years to avoid compressive myelopathy, whereas surgery may be indicated for patients with constant or progressive neurological deficits resulting from spinal cord compression.