Answer of April 2025
For completion of the online quiz, please visit the eHKAM LMS website.
Clinical History:
A 9-year-old boy with a recent history of influenza-like illness one week ago, presented with two-day onset of bilateral loss of vision and weakness of four limbs. Physical examination demonstrated upper motor neuron signs on all four limbs. Plain CT brain was unremarkable. Magnetic resonance imaging (MRI) brain and spine with contrast was performed.
MRI brain and spine with contrast
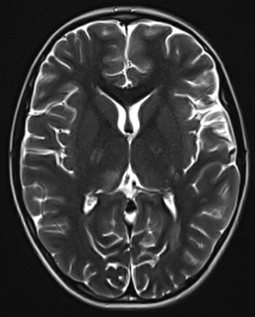
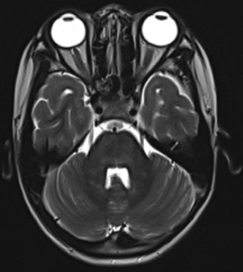
MRI brain T2 weighted sequence - axial
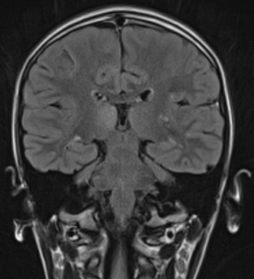
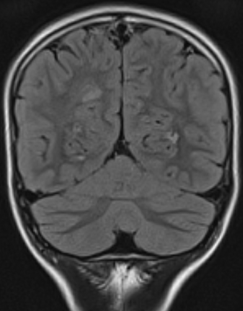
MRI brain T2 weighted FLAIR sequence - coronal
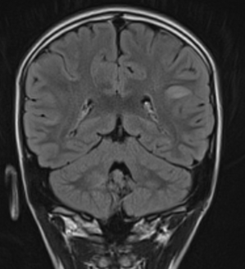
MRI brain T2 weighted FLAIR sequence - coronal
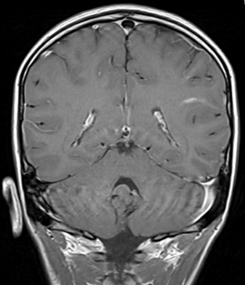
MRI brain T1 weighted sequence with contrast - coronal
MRI brain T2 weighted FLAIR sequence - coronal
MRI brain T2 weighted sequence – axial
MRI cervical spine T2 weighted STIR sequence – sagittal
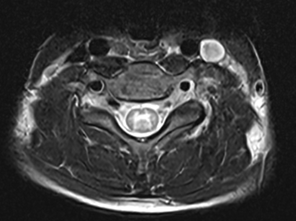
MRI cervical spine T2 weighted sequence – axial
DIAGNOSIS:
Acute disseminated encephalomyelitis.
FINDINGS:
MRI of the brain shows multifocal T2 hyperintense lesions at the subcortical white matter bilaterally with asymmetrical distribution, involving left frontal lobe, bilateral parietal lobes and bilateral occipital lobes. Bilateral temporal lobes are relatively spared. There are also multiple T2 hyperintense lesions at bilateral cerebral peduncles, bilateral internal capsules, and brainstem. T2 hyperintense lesions are also seen involving the deep grey nucleus in particular the right thalamus and to a lesser extent the left thalamus.
Mild enhancement is observed at the left parietal lobe subcortical lesion. There is no associated restricted diffusion, blooming artefact, or mass effect observed.
MRI of the spine shows diffuse involvement of the spinal cord with increased T2 signal and syrinx formation. The spinal cord is swollen particularly at the cervical cord. No associated enhancement is detected.
DISCUSSION:
Acute disseminated encephalomyelitis (ADEM) is a monophasic inflammatory condition of the central nervous system, most commonly affecting young adults and children. It is usually the result of inflammatory response to viral infections and vaccinations. Clinical presentations are non-specific with a wide range of signs and symptoms, such as multifocal neurological symptoms, convulsions, lethargy, and even coma. Cerebrospinal fluid (CSF) tests could show elevated leukocyte and protein levels. In view of the non-specific clinical features and laboratory findings, magnetic resonance imaging (MRI) of the central nervous system would be crucial for narrowing down the differential diagnosis.
MRI of the brain typically demonstrates multifocal T2 hyperintense lesions bilaterally with an asymmetrical distribution. Commonly affected regions include the subcortical white matter, brainstem, middle cerebellar peduncle, and periventricular white matter. Deep gray matter, including the basal ganglia and thalamus, are also frequently involved. These lesions may show associated mass effect and enhancement. The spinal cord may also be involved in some of the patients, with a pattern of longitudinally extensive transverse myelitis. These lesions may resolve upon follow up after treatment with steroids.
Differentiating between ADEM and multiple sclerosis has been challenging due to overlapping of the clinical and laboratory findings. Although there are no pathognomonic imaging signs for either condition, the distribution of the T2 hyperintense lesions may suggest one diagnosis over the other. ADEM typically shows asymmetrical involvement, and may affect the deep gray matter including basal ganglia and thalamus, which are rarely affected in multiple sclerosis. The corpus callosum is usually affected in multiple sclerosis, but not affected in ADEM.
Acute necrotizing encephalopathy is another differential diagnosis, sharing similar clinical and radiological features. Both conditions typically affect pediatric patients, and can have a preceding viral infection followed by neurological symptoms. Acute necrotizing encephalopathy also commonly affects thalamus, cerebral white matter, brainstem, and cerebellar hemispheres. However, acute necrotizing encephalopathy shows symmetrical distribution of the lesions in MRI, whereas ADEM shows asymmetrical distribution. Parenchymal hemorrhage may also be seen in acute necrotizing encephalopathy.
Other differential diagnoses would include cerebral vasculitis secondary to infection, myelin oligodendrocyte glycoprotein antibody disease (MOG-AD), aquaporin-4 antibody neuromyelitis optica spectrum disorder (APQ4-NMOSD), Susac syndrome, etc. They may again share overlapping clinical features, but some may have specific laboratory findings, such as serum AQP4 antibody and serum MOG antibody. Neuroimaging may also bring clues to diagnosis by demonstrating the pattern of involvement of the brain, brainstem, spinal cord, and optic nerves. For instance, involvement of optic nerves may occur in multiple sclerosis, APQ4-NMOSD, and MOG-AD, but less commonly in ADEM.
Currently steroids are used in the treatment of ADEM. Patients with ADEM usually have good prognosis, and can generally recover completely with resolution of the central nervous system lesions. Multiple sclerosis has to be considered if the patient does not have a monophasic clinical course, or there is development of new lesions upon long-term follow up.
In summary, inflammatory conditions of the central nervous system could be difficult to diagnose due to overlapping clinical features and laboratory findings. By recognizing the neuroimaging patterns of different diseases, radiologists could play an essential role in narrowing down the differential diagnosis.