Answer of May 2022
For completion of the online quiz, please visit the HKAM iCMECPD website: http://www.icmecpd.hk/
Clinical History:
5 years old boy with unremarkable past health presented with per rectal bleeding with large amount of blood-stained stool. There is history of on and off central and lower abdominal pain. Abdominal exam was unremarkable. On admission there was anaemia with haemoglobin level of 8.9 g/dL.
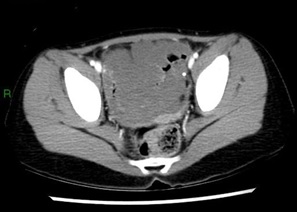
Axial CT pre-contrast
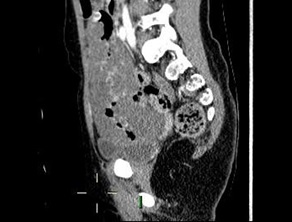
Axial CT post-contrast, portovenous phase
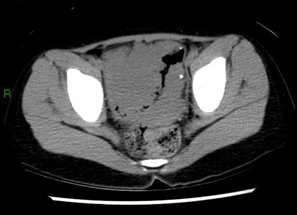
Sagittal reformat CT pre-contrast
Sagittal reformat CT post-contrast, portovenous phase
Coronal reformat CT pre-contrast
Coronal reformat CT post-contrast, portovenous phase
IMAGING FINDINGS
CT shows a long segment of irregular, marked, wall thickening of the small bowel. Portovenous phase images show curvilinear enhancement of the mucosa only. No associated bowel obstruction. Phleboliths are noted in the lesion.
DIAGNOSIS
Vascular malformation of the bowel
ADDITIONAL INFORMATION
The above patient also underwent ultrasound, which revealed a multicystic structure in the lower abdomen with internal echoes and septations (Figure 1 & 2).
(Figure 1. Ultrasound of the lesion in our patient reveals a multicystic appearance of bowel wall thickening. Low level internal echoes are seen.)
(Figure 2. Ultrasound of the lesion in our patient reveals a multicystic appearance of bowel wall thickening. Low level internal echoes are seen.)
The patient underwent laparoscopy converted open resection of the lesion with an unremarkable post-operative course of recovery. The final pathology was signed out as vascular malformation.
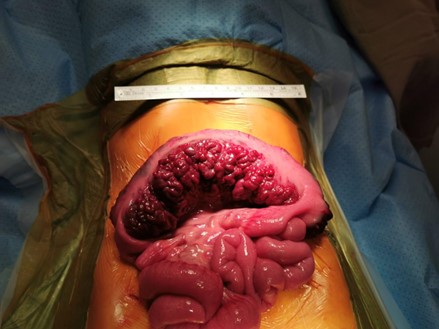
(Figure 3. Intraoperative photo of the patient showing the vascular malformation in distal ileum.)
DISCUSSION
The aetiology of gastrointestinal bleeding differs by age group. Some causes to consider in a preschool child would include intussusception, Meckel’s diverticulum, infective enterocolitis, Henoch-Schönlein purpura, and bleeding diastasis (list is not exhaustive), while small bowel vascular malformation is a rare cause of gastrointestinal bleeding in the paediatric population [1]. In particular, there are only a limited number of reported cases of long segment vascular malformation of the small bowel.
International Society for the Study of Vascular Anomalies (ISSVA) classifies vascular anomalies into vascular tumours and vascular malformations [2]. Amongst vascular malformations they are further divide into simple (slow flow: capillary/ lymphatic/ venous malformations; high flow: arteriovenous malformations or arteriovenous fistula), combined (two or more of the above vascular malformations in one lesion), anomalies of major named vessels, and those associated with other anomalies.
Expected imaging appearances of venous malformation on CT include low attenuation bowel wall thickening with or without phleboliths and delayed contrast enhancement, while that of arteriovenous malformation would include presence of feeding artery/arteries, draining vein(s), and vivid enhancement of the lesion itself.
Other modalities of imaging may also aid in tissue characterization and ruling out other pathologies. Ultrasound is important to rule out more common causes in the same demographic, in particular intussusception. In the limited reports of ultrasound performed in cases of vascular malformation of the bowel, there is common description of cystic components in keeping with the vascular spaces [3,4]. Doppler colour signal may be detected in high flow lesions and absent in slow flow lesions. Pseudo-flow, however, may be elicited in slow flow lesions [4].
Treatment depends on size and type of lesion. Small haemangiomas may be treated conservatively with medical and supportive treatments. Medications involved include corticosteroid, antiangiogenic agents, interferon alpha, while supportive measures include transfusion and iron supplements [5]. For lesions not responsive to medical treatment, large lesions, and symptomatic lesions causing severe GI bleeding, further intervention (sclerotherapy, embolisation, and resection) should be considered.