Answer of November 2021
For completion of the online quiz, please visit the HKAM iCMECPD website: http://www.icmecpd.hk/
Clinical History:
49-year-old male with DM and hypertension and
otherwise unremarkable past medical history.
Admitted for ankle sprain sustained when falling on the stairs. Reported
landing with foot inverted. Developed pain and swelling afterwards with
inability to bear weight. X-ray and CT
were performed.
IMAGING FINDINGS:
X-ray and CT show medial and posterior malleolar non-displaced fractures, with absence of an apparent fibular fracture.
Subtle widening medial tibiotalar clear space (XR,CT) and syndesmosis (CT) are present, indicating deltoid and syndesmotic ligament injuries, respectively.
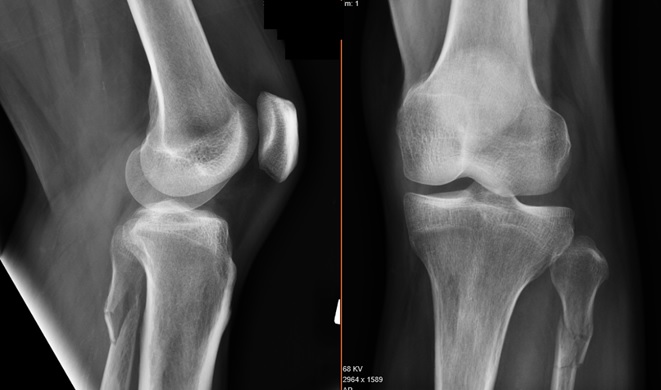
Maissoneuve fracture was suspected on the basis of the above combination of findings (medial malleolar fracture WITHOUT lateral malleolar fracture), and suggestion was made for radiographs of the leg/knee were made. These showed a proximal third fibular fracture, confirming the diagnosis of Maissoneuve fracture (see X-ray below).
DIAGNOSIS:
Knee radiograph
DISCUSSION:
Maissoneuve fracture is a classic injury described by 17th century surgeon Jules Maissoneuve, and is a combination of a proximal third fibular fracture (Weber C) with an unstable ankle injury. It results from pronation (eversion)-external rotation mechanism to the ankle with transmission of the force through the interosseous membrane, which exits in a proximal third fibular fracture. The syndesmosis and deltoid ligaments are injured in the process.
Ankle radiographs and CT show a medial malleolar fracture +/- a posterior malleolar fracture, in the absence of a distal fibular fracture. Widening of the syndesmosis may be present but can be subtle and difficult to detect. The diagnosis is easily overlooked by the unwary surgeon and radiologists, as the patient presents with an ankle injury with paucity of signs referable to the upper leg and knee. More experienced clinicians and radiologists, on visualizing a medial malleolar fracture without an apparent lateral malleolar fracture, should recognize a red flag for the diagnosis of Maisonneuve injury and suggest radiographs of the proximal leg / knee to visualize the fibular neck fracture.
The importance of recognizing the Maisonneuve fracture lies in its impact on management decision-making, since there is a high risk of associated syndesmotic instability. The patient should be examined under anaesthesia to assess the degree of syndesmotic stability. Most surgeons will prefer operative management with at least two long syndesmosis screws, while a few surgeons may opt for immobilization with a long leg cast if the syndesmosis is well-aligned and stable although this carries a risk of subsequent displacement and resultant ankle instability.