Answer of July 2021
For completion of the online quiz, please visit the HKAM iCMECPD website: http://www.icmecpd.hk/
Clinical History:
A 74 year-old male was admitted for abdominal distension, pain and no bowel opening for 2 weeks. There is no nausea or vomiting. Abdominal examination revealed no localizing peritoneal sign, but hyperactive bowel sounds. Abdominal radiograph and urgent computed tomography (CT) of abdomen & pelvis with contrast were arranged.
IMAGE FINDINGS:
The abdominal radiograph on admission shows mildly prominent, fecal-loaded large bowel loops. No pneumoperitoneum was evident.
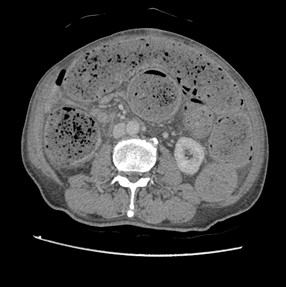
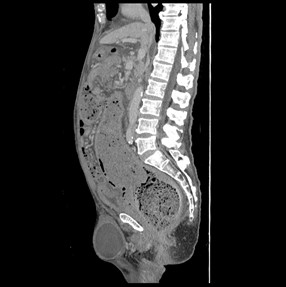
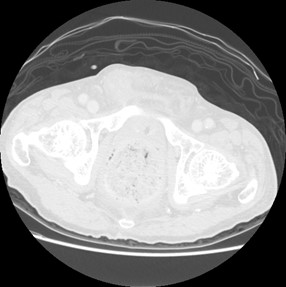
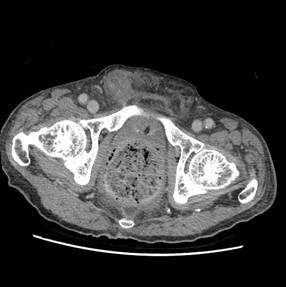
The CT shows dense fecal material at rectum is suggestive of fecaloma, with proximal mildly dilated large bowel loops. Small bowel loops were not dilated and closed-loop obstruction is suggested. No obstructive colonic mass is seen. Significant diffuse rectal wall thickening and perirectal fat stranding are present. Tiny gas locules seen at the rectal wall are suspicious of intramural gas.
No portal venous gas nor pneumoperitoneum was evident. Overall features are suggestive of stercoral colitis.
An incidental postoperative seroma for right hernioplasty is also included at sagittal image.
DIAGNOSIS:
Stercoral colitis
DISCUSSION:
Stercoral colitis is a rare form of inflammatory colitis related to increased intraluminal pressure from impacted fecal material in the colon. It can lead to serious complications such as colonic perforation and death. When stercoral colitis is associated with colonic perforation, a 35% mortality rate has been reported due to life-threatening fecal peritonitis.
Fecal impaction leading to colonic obstruction is seen primarily in the elderly, often those who live in nursing homes or, less often, young patients who are neurologically impaired. There is also an association with medications that slow down bowel transit (e.g. opiates, tricyclic antidepressants, and tranquilizers).
Chronic constipation & fecal impaction can lead to formation of fecaloma, which is a conglomeration of dehydrated fecal material. This causes colonic luminal distention and increases the pressure on the wall, which then decreases blood supply. This further results in ulceration leading to colonic perforation.
The most common locations of ulceration are in the sigmoid colon and the rectum. It favours the antimesenteric side of the bowel wall, due to relative poorer blood supply to this side.
Imaging findings that should prompt the radiologist to consider this diagnosis are the presence of fecal impaction or fecaloma, focal colonic wall thickening (representing edema from ischemia and ulceration), and adjacent pericolonic or perirectal fat stranding (suggesting colonic/ rectal edema or ischemia). Radiologists should then pay attenuation to look for extraluminal gas bubbles or an abscess suggests that perforation has already occurred.
It should be emphasized that a differentiation from constipation should be made. First, in uncomplicated fecal impaction, the colon is distended and the wall is thin. Second, there should be no pericolonic or perirectal fat stranding. Third, no extraluminal gas locules, abscess nor pneumoperitoneum should be seen.
Important laboratory findings to highlight are elevated lactic acid and anion gap metabolic acidosis in the setting of stercoral colitis, this should raise concern for bowel ischemia or perforation. It has been suggested that elevated lactic acid level secondary to ischemia of the bowel wall with CT scan findings aid in establishing the diagnosis of stercoral colitis complicated with ischemic colitis. And urgent & aggressive treatment with laxatives and fecal disimpaction is indicated at this stage to prevent perforation and peritonitis.
Besides, patients can develop sepsis and septic shock in severe cases, so blood cultures and preoperative labs such as type and screen and coagulation panel should be obtained
Patients who do not show signs of peritonitis can be managed non-operatively with manual disimpaction via the rectum or with endoscopically guided disimpaction, bowel regimen, and admission for close monitoring. If frank perforation occurs, fecal material is found within the peritoneal cavity in close proximity to the perforation site. Treatment is usually resection of the affected bowel, colostomy, and Hartmann's pouch.
For our case, the patient was initially treated with aggressive laxatives (including fleet enema) and digital evacuation with minimal bowel opening. Colonoscopic decompression was performed subsequently, and underlying obstructive lesions are also excluded in the same setting.
In summary, it is important for radiologists to recognize this condition, as well as the potential serious clinical implications of the condition. The imaging findings of colonic wall thickening and pericolonic fat stranding suggest colitis. When associated with fecal impaction and in the right clinical setting, these findings should suggest stercoral colitis. Timely and appropriate management to relive faecal impaction could be offered to prevent the serious complications and death.