Answer of September 2020
For completion of the online quiz, please visit the HKAM iCMECPD website: http://www.icmecpd.hk/
Clinical History:
A 52 year-old woman presented with progressive swelling of the left lower limb for a few weeks. There was no history of injury to the left lower limb. No skin wound nor overlying skin change is noted. She had not taken any over-the-counter medicines recently. She was stable and afebrile at the time of examination.
An urgent Doppler Ultrasound study of the left lower limb was arranged and found extensive left deep vein thrombosis. She was started on subcutaneous low-molecular weight heparin (Enoxaparin) therapy.
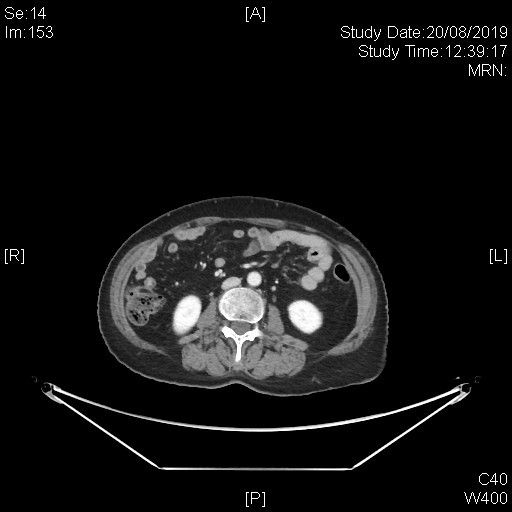
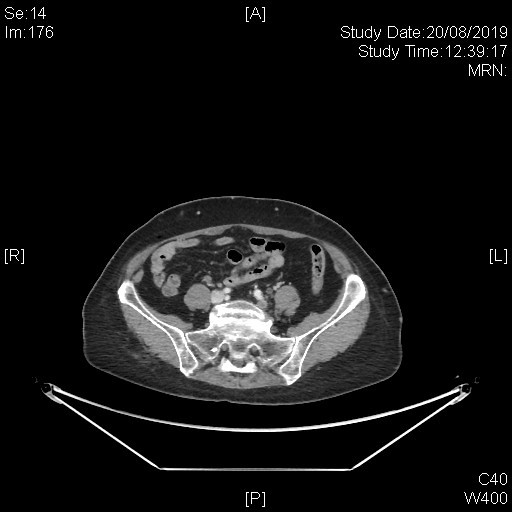
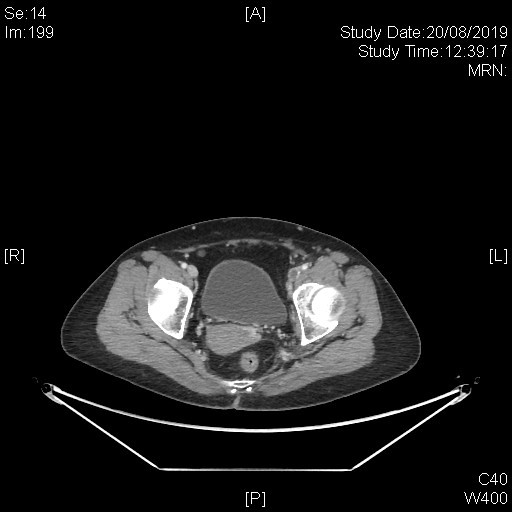
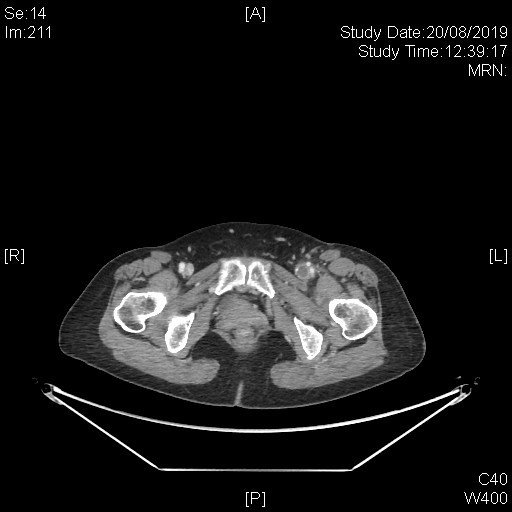
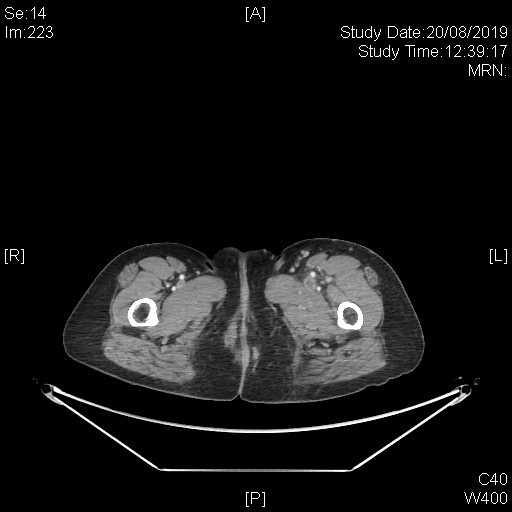
A subsequent whole body PET-CT study with IV contrast was done with excerpts of the post-contrast CT images as shown below.
Imaging Findings:
This series of captured axial CT images from the abdomen and pelvis of this patients shows a “slit-like” configuration of the origin of the left common iliac vein when compared to the right. It is compressed between the right common iliac artery and the vertebral body at its original expected location. The included distal left common iliac vein and superficial femoral vein are dilated with intraluminal filling defect in keeping with underlying thrombosis. This is consistent with May-Thurner Syndrome causing left-sided deep vein thrombosis.
Diagnosis:
May-Thurner Syndrome
Discussion:
May-Thurner syndrome refers to the compression of the left common iliac vein by the right common iliac artery against the vertebral body. It is not an infrequent finding in patients with imaging studies done for other indications, with one retrospective study showing 24% of patients had greater than 50% compression of the left common iliac vein. Not all patients are symptomatic and the onset of the venous thrombosis is often seen around the 4th decade of life, with a predilection in women and risk factors similar to that venous thrombosis such as immobilization. It is proposed that venous stasis is a result of venous intimal injury and chronic fibrous adhesion due to repetitive injury from the arterial pulsations against the bony vertebra.
In addition to the imaging finding of left common iliac vein compression, other causes of deep vein thrombosis such as pelvic mass or malignancy and primary hypercoagulopathy should be excluded before the diagnosis of May-Thurner Syndrome is made.
Various imaging modalities can be used to aid the diagnosis, including color Doppler imaging, intravenous contrast Ultrasonography, CT venography or MR venography. Digital subtraction angiography has widely been considered the gold standard for diagnosis. The procedure can demonstrate the degree of the left common iliac vein stenosis and also visualize any pelvic venous collaterals, which is an indication of hemodynamically significant compression.
Treatment of May-Thurner Syndrome includes administration of anticoagulant to prevent distant embolism of the venous thrombosis. However, due to the mechanical nature of the disease, patients generally do not respond well to solely anticoagulation. Definitive treatment to prevent recurrent venous thrombosis includes surgical treatment, which in the past resulted in variable outcomes. Endovascular intervention, including angioplasty and stent placement, is now the treatment of choice. Catheter-directed thrombolysis or mechanical thrombectomy can also be performed in combination if vein thrombosis is present.