Answer of January 2017
For completion of the online quiz, please visit the HKAM iCMECPD website: http://www.icmecpd.hk/
Clinical History:
A 68-year-old woman with history of frequent falls. Physical examination shows atrophy of left side of tongue. MRI brain and neck images are shown.
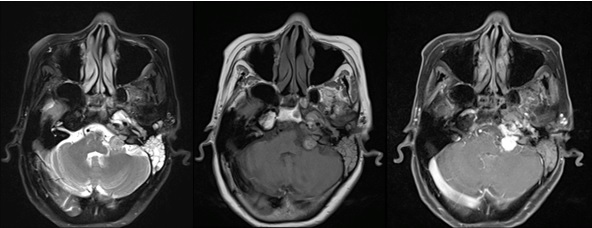
Figure 1. MRI (T2W, T1W, T1W post-contrast)
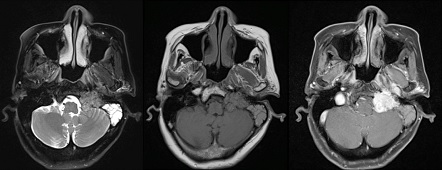
Figure 2. MRI (T2W, T1W, T1W post-contrast)
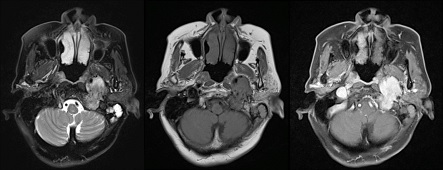
Figure 3. MRI (T2W, T1W, T1W post-contrast)
Imaging Findings:
A large T1 isointense T2 intermediate signal tumour is seen extending from left cerebellopontine cistern to left carotid space. There is marked expansion of both endocranial and exocranial left jugular foramen with involvement of left hypoglossal canal. Several high velocity flow voids are seen within the tumour. Uniform intense enhancement is seen after contrast. There is no dural tail.
Diagnosis:
Glomus jugulare paragangliom
Discussion:
Glomus jugulare paraganglioma are rare tumours, but it is the most common jugular fossa tumour. It is typically seen in adults, typically between 40 and 60 years of age, with a moderate female predilection.
Clinical presentation depends on degree of middle ear involvement. Common presentations include pulsatile tinnitus and hearing loss. Other presentations include lower cranial nerve palsies, more commonly facial nerve palsy.
A typical imaging description of this tumour is that it has a salt and pepper appearance on both T1 and T2 sequences ; the salt representing blood products from haemorrhages or slow flow and the pepper representing the flow voids due to high vascularity.
It is a slow growing tumour. Average time from onset of symptoms to treatment is 3 years. Skull base paragangliomas are radiosensitive when compared to their cervical counterparts such as carotid body tumours which are relatively radioresistant, thus large inoperable tumours or tumours in elderly and frail patients are often treated with radiotherapy if they are not fit for surgery.
Recurrence and local invasion is common, occuring in up to about half of the cases.