Answer of June 2016
For completion of the online quiz, please visit the HKAM iCMECPD website: http://www.icmecpd.hk/
Clinical History:
A baby girl was delivered via LSCS due to pathological cardiotocography, at 41 weeks of gestation. The birth weight was 3.27kg. The umbilical cord was seen round the right foot, but not round the neck. The Apgar score was 6, 7 and 10 at 1, 5 and 10 minutes respectively. There were several episodes of seizures on the first few days of life, presented with twitching of upper and lower limbs and abnormal eyeblinking. There were also few episodes of transient breath holding with desaturation. CT and MRI brain were arranged when she was 3 days old. Follow-up MRI brain was performed when she was 25 days old.
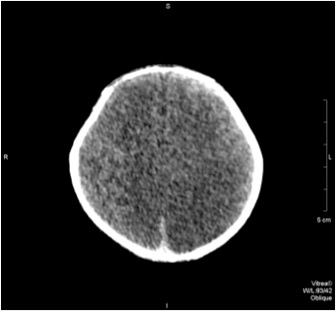
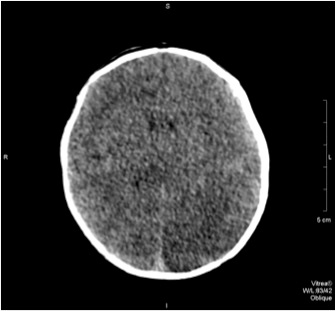
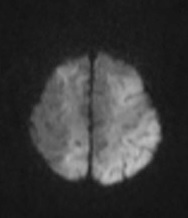
CT scan
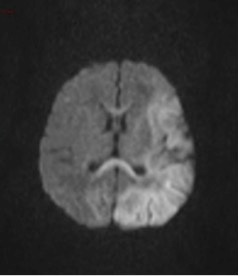
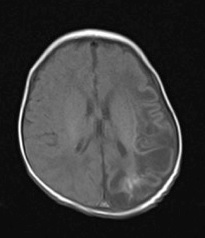
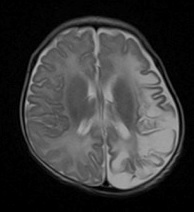
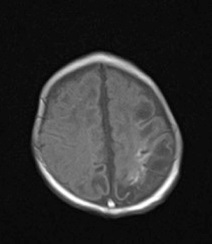
MRI scan on 3 days old
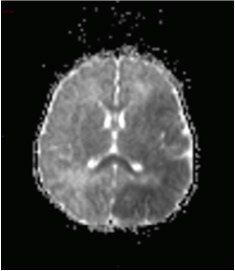
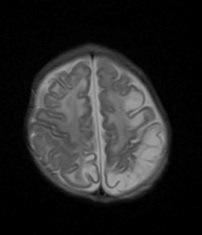
MRI scan on 25 days old
Diagnosis:
Hypoxic ischemic encephalopathy
Discussion:
Hypoxic ischemic encephalopathy (HIE) is a major cause of death and neurodevelopmental disability in term neonates. The prevalence of HIE is between two and four per 1000 live term births. Between 15% and 20% of infants suffering from HIE die during the neonatal period. An additional 25% develop permanent neurological deficits, including cerebral palsy, mental retardation and epilepsy.
Clinical signs and symptoms of neonatal HIE are non-specific at birth, including intrapartum distress (fetal heart rate abnormality), severe functional depression (indicated by a low 5-minute Apgar score), severe fetal acidemia, abnormal early neurologic examination and abnormal electroencephalogram.
Imaging features are highly variable, depending on the brain maturity, severity of asphyxia and duration of insult. For neonates who suffer from mild to moderate hypoperfusion (partial asphyxia), blood flow is redistributed to metabolically active grey matter such as basal ganglia, brainstem and cerebellum. On the contrary, the metabolically active grey matters are affected in neonates with severe hypoperfusion (severe asphyxia).
In term neonates with severe asphyxia, ultrasound shows obliteration of CSF spaces suggestive of cerebral edema and increased echogenicity at basal ganglia, thalamus and brainstem. Restricted diffusion is seen in the basal ganglia with sparing of the cerebral cortex on MRI scan. In term neonates with partial asphyxia, the cerebral cortex and white matter at watershed area are most affected, with cortical swelling and loss of grey-white matter differentiation seen.
The injury patterns of severe asphyxia in preterm neonates are similar to those in term neonates. However, there are characteristic features in preterm neonates that could help differentiate from those in term neonates, including occurrence of germinal matrix hemorrhage with periventricular leukomalacia and relative sparing of the perirolandic cortex. Periventricular leukomalacia are sometimes seen in preterm neonates with partial asphyxia, with cavitation and periventricular cyst formation between 2 to 6 weeks after the insult. Ventriculomegaly, irregular margin of lateral ventricles and thinning of corpus callosum are the features of end-stage periventricular leukomalacia.