Answer of April 2016
For completion of the online quiz, please visit the HKAM iCMECPD website: http://www.icmecpd.hk/
Clinical History:
A 13 years old boy with good past health presented as left shoulder mass for several years without any pain. The mass was gradually increasing in size. He has strong family history of bony masses. His father had history of bony mass excision in his teenage. Physical examination found 4cm diameter bony mass on the lateral aspect of left upper arm. Range of movement of his left shoulder was full.
Work up includes plain radiographs of his left humerus (Picture 1-2) and subsequent MRI (Picture 3-8).
Picture 1
Picture 2
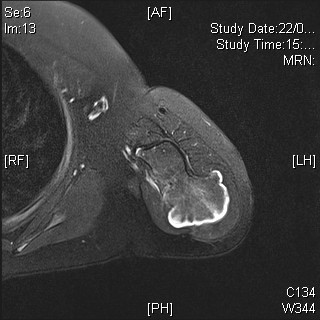
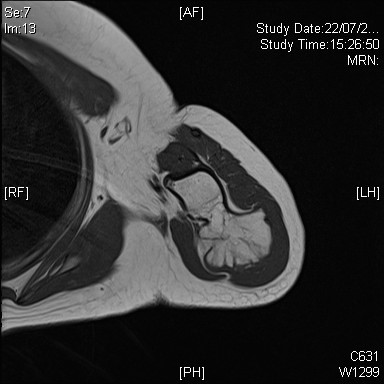
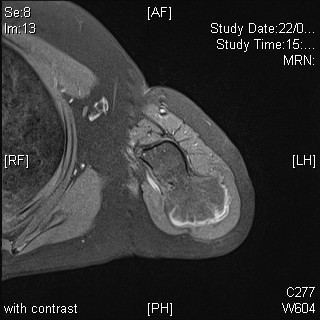
Picture 3 (Axial T2 with fat saturation)
Picture 4 (Axial T1)
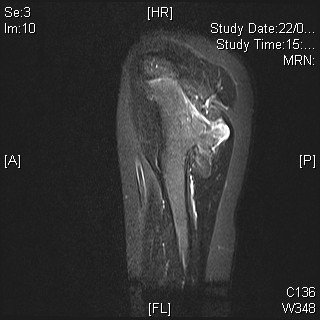
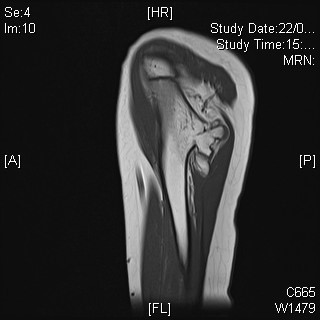
Picture 5 (Sagittal STIR)
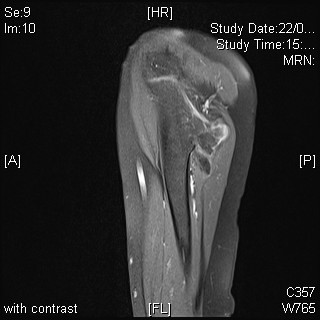
Picture 6 (Sagittal T1)
Picture 7 (Axial T1 post-gadolinium)
Picture 8 (Sagittal T1 post-gadolinium)
Imaging Findings:
In plain film, there are two well-defined broad-based protrusions at metadiaphyseal region of proximal humerus, continuous with the parent cortex and trabeculae. The lesions are directed away from the shoulder joint. No associated fracture is noted. Soft tissue bulging conforming the bony protrusions are noted but there is no added soft tissue mass. No phleboliths noted.
Diagnosis:
The
overall imaging findings and the strong family history are in keeping with
diaphyseal aclasis. Surgical excision of the lesion was performed for the
largest lesion due to cosmetic reason and confirmed osteochondroma with no
sarcomatous change.
Discussion:
Osteochondroma is the most common bone tumour, typically manifests in first to second decades of life. It stops growing when the nearest epiphysis fused. The tumour usually occurs in metaphyseal region of long bones. Distal femur, proximal tibia, proximal humerus, pelvis and scapula are common occurring sites. When there are multiple osteochondroma, the condition is termed multiple hereditary exotosis or diaphyseal aclasis, which is an autosomal dominant condition.
On plain film, osteochondroma is a well-defined eccentric protrusion continuous with the parent bone cortex and trabeculae. It can be pedunculated with a narrow stalk, or sessile with a broad base. It is usually directed away from the nearest joint and migrates away from the end of the bone as growth proceeds. The cartilage cap is usually not visible on plain film in young age, and becomes mineralized in adult, giving and arcs and rings appearance or flocculent calcifications.
MRI is the best imaging modality to demonstrate cortical and medullary continuity between the tumour and parent bone. On MRI, thin hyaline cartilage cap of low to intermediate signal on T1 sequence and high signal on T2 sequence reflects its high water content. Its mineralized area would be low signal at all sequences. Slight septal and peripheral enhancement can be present.
Complications of osteochondroma include cosmetic deformity, fracture, vascular compromise causing occlusion or pseudoaneurysm formation, nerve compression, bursitis and malignant transformation into chondrosarcoma. If there is history of rapid growth of a stable lesion or continued growth of the lesion after skeletal maturation, malignant transformation should be considered. Other features of malignant transformation also include onset of pain without any fracture and cartilaginous cap of more than 1.5cm thick. The risk for a solitary osteochondroma to become malignant is less than 1%, but the risk can be up to 5-25% for multiple osteochondromas.