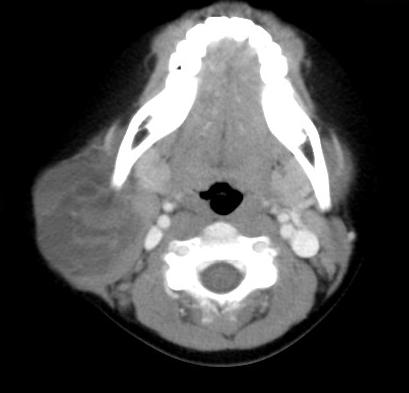
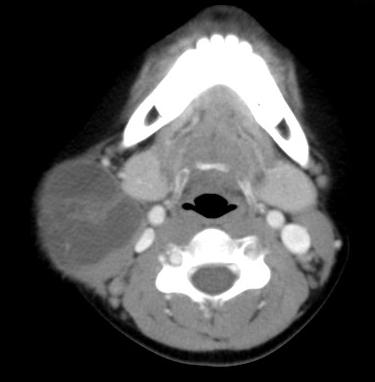
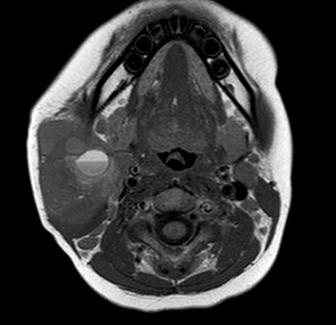
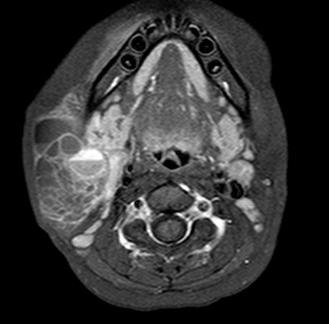
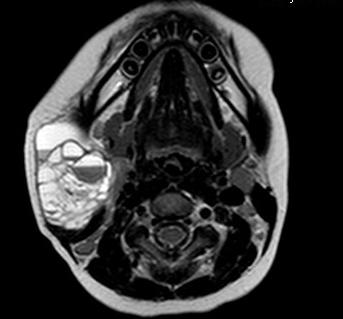
CLINICAL HISTORY: DIAGNOSIS: DISCUSSION: Lymphangioma can be associated with chromosomal abnormalities in 60-80% of cases, for example Turner syndrome or trisomies 13, 18, 21 etc. It is also believed to be associated with exposure to teratogens such as fetal alcohol syndrome or aminopterin. Patient is usually presented with asymptomatic soft or semi-firm mass over the neck, however the mass can show rapid increase in size due to infection or haemorrhage. In some cases, patient may presents with dyspnea or dysphagia if the mass is large enough with encroachment upon trachea, pharynx or esophagus. On USG scan, there would be thin-walled fluid-filled structures with multiple septa of variable thickness and solid cyst wall components. It can be easily recognized by fluid-fluid levels with layering of haemorrhagic component. CT scan and T2W MRI images also revealed multiloculated septated cystic cavities with fluid-fluid levels. Hyperintense signals on T1W images are likely due to clotted blood or high chylous lipid content. It can be differentiated from other masses by its location and characterized fluid-fluid levels with previous haemorrhage, and be differentiated from haemangioma by lack of contrast enhancement and feeding vessels. |
||
PREVIOUS CASES |
||
HOME |
COMMENTS |
|