CLINICAL HISTORY:
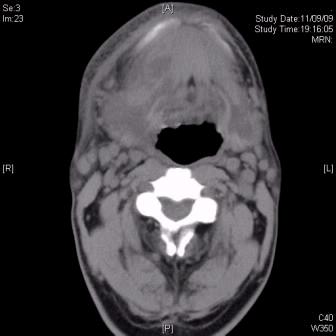
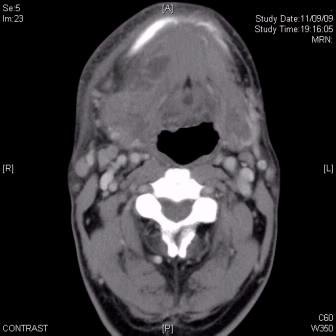
A 56 year-old gentleman presented with fever and swelling over the right submental and submandibular region. He was a known diabetic. Radiograph of the neck was unremarkable. Computed tomography (CT) of the neck was performed.
DIAGNOSIS:
Ludwig’s angina (Extensive infection of the floor of the mouth).
DISCUSSION:
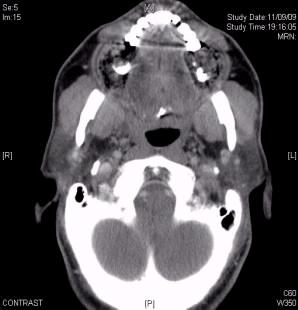
Computed tomography shows an irregular cystic lesion in submental, right sublingual and right submandibular spaces. It demonstrates vague ring-enhancement and a homogeneous center with fluid density. It locates inferior to the mandibular body, and tracks irregularly into the right sublingual and submandibular spaces. Both submandibular glands are diffusely swollen but no intraglandular mass was noted. Amorphous gas densities are noted around bilateral premolar regions of the upper jaws (fig.5), indicating concurrent dental infection.
The term Ludwig’s angina refers to an extensive infection of the floor of the mouth, predominantly caused by oral flora (especially streptococcal and staphylococcal bacteria). Polymicrobial infection occurs in over 50% of cases. Most cases are of odontogenic origin, in which infections of mandibular molars account for up to 90% of reported cases. Less common causes include peritonsillar or parapharyngeal abscess, epiglottitis, and penetrating injuries to the floor of mouth. Bad dentition or impaired immune function such as diabetes mellitus, HIV, alcholism are recognized risk factors.
Patients may present with sublingual or submandibular swelling, painful tongue with dysphagia, dysphonia, elevation and backward displacement of tongue causing airway compromise. Before the antibiotic era, aggressive infections in floor of the mouth dissect inferiorly along fascial planes into mediastinum, angina-like chest pain resulted and thus named.
Ludwig’s angina describes a progressive gangrenous cellulitic condition. The clinical criteria for diagnosis include: 1) involves both the sublingual and submandibular spaces, and frequently bilateral; 2) produces gangrene or serosanguious phlegmon yet little frank pus; 3) involves connective tissue, fascia, and muscle but not glandular structures; and 4) spreads by contiguity instead of lymphatic. However, reactive or suppurative adenopathy involving the submandibular and submental lymph nodes are commonly seen in association with oral cavity infections or as part of a more systemic inflammatory response.
The principle role of imaging is to evaluate the patency of airway, document the presence of underlying dental infection, and look for possibly drainable neck abscesses. Complications such as mandibular osteomyelitis and infection of carotid sheath structures should not be overlooked. Contrast-enhanced CT hence is the study of choice.
The definitive treatment of Ludwig’s angina involves early airway protection (intubation or if fails, tracheotomy), and a combination of broad-spectrum antibiotics with surgical decompression of the firmly indurated submandibular space. With timely aggressive management, the mortality of Ludwig’s angina has been reduced to less than 10%. |