CLINICAL HISTORY:
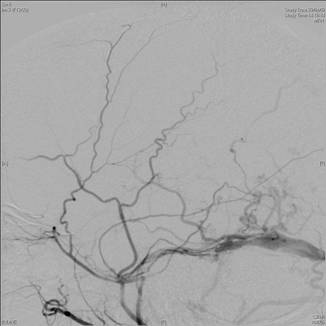
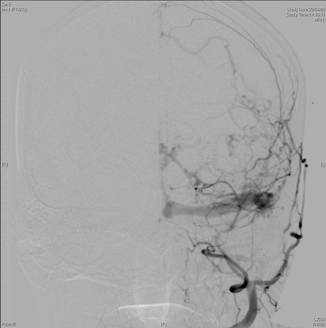
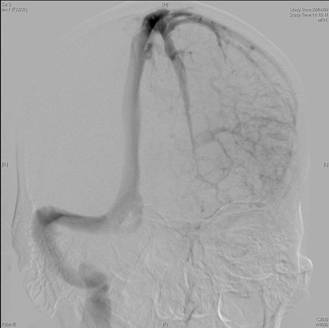
A 52year old man presented with acute confusion. Plain CT brain and subsequent cerebral angiography (left ECA and left ICA venous phase shown) were performed.
DIAGNOSIS :
Dural arteriovenous fistula
DISCUSSION:
Plain CT brain shows left basal ganglial parenchymal hemorrhage, bilateral intraventricular hemorrhages more on the left, and subarachnoid hemorrhage over the left Sylvian fissure.
Cerebral angiogram shows a left dural arteriovenous fistula receiving multiple arterial feeders from left ECA dural branches. The left sigmoid sinus is occluded and retrograde drainage into the left transverse sinus is noted. Retrograde drainage into the left cortical veins and left medullary veins are also present (not shown).
Intracranial dural arteriovenous fistulas (dAVF) are believed to be an acquired condition. They account for 10-15% of all intracranial vascular malformations. The most frequent sites are at the transverse, sigmoid and cavernous sinuses.
Clinical presentation is varied, ranging from asymptomatic, to minor symptoms such as headache, tinnitus and visual symptoms, to aggressive presentations such as neurological deficits and intracranial hemorrhage. Intracranial hemorrhages are attributed to venous hypertension, which cause rupture of congested cortical and/or subependymal veins, resulting in subdural, subarachnoid, parenchymal or intraventricular hemorrhages or in various combinations.
The pattern of venous drainage of dAVF is the most predictive factor of the risk of aggressive presentation, with retrograde cortical venous drainage showing the highest risk and antegrade sinus drainage the least risk.
The best imaging modality is cerebral angiography. Typical findings are multiple arterial feeders arising from dural branches from the ECA (less commonly ICA tentorial branches), arterial inflow into a common recipient pouch, and drainage either antegrade or retrograde into a dural sinus or cortical or medullary veins. Frequently, the involved dural sinus is thrombosed and occluded. A pseudophlebitic pattern correlating with venous congestion may also be seen over the cortical veins.
Management is with a multidisciplinary team, and depends on clinical presentation, location and type of the dAVF. Treatment modalities include endovascular intervention, radiation therapy, surgery, or a combination. Excellent results with a low complication rate have been reported.
|