|
|
XR-LS-spine (frontal) |
|
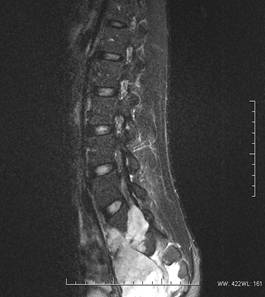
MRI
T1W Sagittal |
|
T2W Fat suppression Sagittal |
|
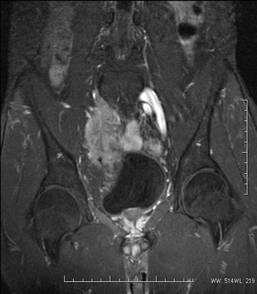
T2W FS Coronal |
|
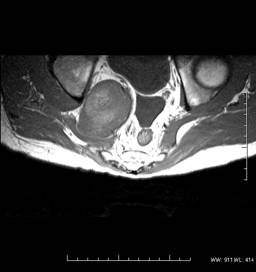
T1W Axial
| |
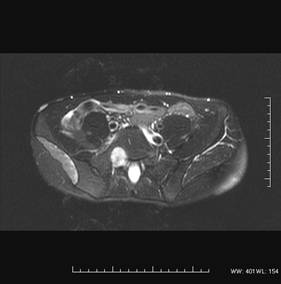
T2W FS Axial
| |
CLINICAL HISTORY: A 33 years-old-man presented with 6-months history of low back pain and right lower limb weakness. There was no fever, constitutional symptoms or previous traumatic insult. Physical examination was unremarkable. No lower limb neurology or sphincter disturbance. He had past history of pineal germinoma at the age of 17, and was treated with debulking surgery and RT(cranial and spinal). Currently the disease was in remission. Plain radiographs and MRI of the lumbar spine were performed. RADIOLOGICAL FINDINGS: X-ray-
MRI-
DIAGNOSIS: DISCUSSION: MPNST represents 5-10% of soft tissue sarcomas, and usually affects patients in the age range of 20-50. A high proportion (~50%) of MPNST occurs in association with patients with NF-1. On the contrary, only 5% of NF-1 patients would develop MPNST. There are two forms of MPNST: primary and secondary (related to previous irradiation, with latency period of ~10 years). It is usually the larger major nerve trunks being involved. Radiologically, there is no absolute reliable criteria in differentiating benign and malignant peripheral nerve sheath tumour.
The prognosis of MPNST is dismal. Local recurrence is common. Treatment usually entails a combination of surgery, irradiation and chemotherapy. |
||
PREVIOUS CASES |
||
HOME |
COMMENTS |
|