| |
Plain Contrast |
|
This is the patient.s chest X ray. CT thorax with contrast was performed as an abnormality is noted on CXR. | |
MIP images from CT thorax with contrast | |
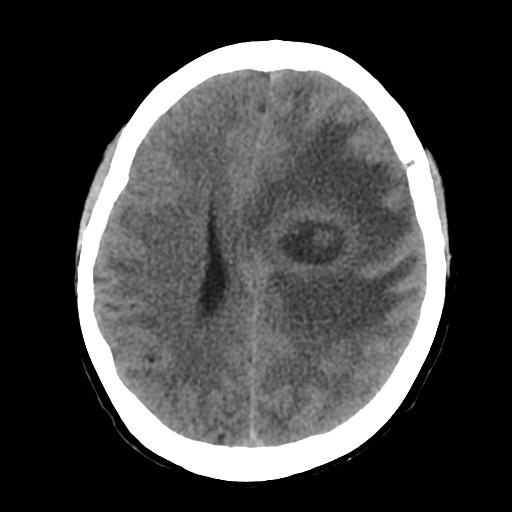
CLINICAL HISTORY: DIAGNOSIS: DISCUSSION: Patients with PAVF are usually asymptomatic till adulthood (3rd or 4th decade). CNS symptoms are commonly the initial manifestation, like cerebrovascular accident (ischemic stroke, TIA) and brain abscess, due to absence of filter effect of capillaries in pulmonary circulation on emboli or septic emoboli. Sometimes patient may have chest symptoms, like hemoptysis, shortness of breath, especially if there are multiple PAVF or if they are large, which produces right to left shunt and hypoxia. |
||
PREVIOUS CASES |
||
HOME |
COMMENTS |
|